Zero-based licensing would restore loyalty to patients, heal patient-clinician relationships, unleash professional growth, and reduce healthcare costs. Think of it as a state licensing reset.
Licensing history
A majority of the members of an appointed examining or licensing board of a profession shall be members of that profession.
– Michigan Constitution Article V, Section 5
The unfortunate effect of professional control has been limited entry to the professions, rather than abundant healthcare. This impacts all of us straight in the wallet, and in our care.
Under healthcare licensing laws, the state sets targeted limits on practice. Obnoxiously, Michigan restricted access to COVID treatment when it threatened physician and pharmacist licenses. Ongoing denials of effective treatment for chronic pain patients also come down to license threats.
Expensive care is the result. One study found that licensing stringency is associated with higher prices, especially for expensive jobs: a 21.4% increase per $1000 or more.
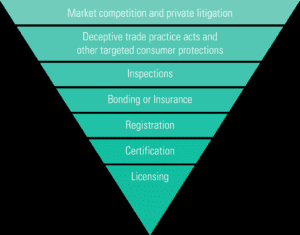
Factoring such costs into every bill analysis might help. Traditional licensing reforms include using:
- less-restrictive means
- regular legislative review
- universal licensing
- expanding scope of practice
Each measure pulls a thread from the licensing tangle. Unfortunately, the core problem continues. Michigan licensing just keeps splitting off in new directions, getting more and more complicated and expensive.
Every year legislators propose more specialty licenses and tweak others, most recently here, here, here, and here.
It’s time to reset to freedom with zero-based licensing.
Zero-based licensing
Zero-based licensing limits the state to issuing a base license for a health profession, with renewals. No specialty licenses or certificates, no CE mandates, no state records of ongoing education. Disciplinary hearings would be related to patient harm, only.
No licenses for non-professions (that is, occupations that don’t formally self-educate at the college level).
This concept simplifies Michigan law, restores the patient-clinician relationship, and reduces healthcare costs for patients and taxpayers.
How would zero-based licensing look?
A nursing student graduates, passes the national test, and applies for a state license.
Currently, the nurse faces additional state barriers for any specialty she may wish to pursue: clinical nurse specialist (CNS), nurse practitioner (NP), nurse anesthetist (CRNA), certified nurse midwife (CNM), etc. Each license has its own fees and continuing education requirements.
Under zero-based licensing, these specialties would require only completing further education, with optional national organization certification. As in the current medical licensing model, specialists would have no additional state requirements or scope of practice limits.
Who Wins
Zero-based licensing sweeps away artificial scope of practice restrictions, removes silos, promotes collegiality among the professions, and yields more comprehensive care for patients. All are especially important in rural areas with fewer specialists.
This simplified structure puts professionals in charge of their practice, and makes them responsible for further education and training to best serve their patients. In addition, they will be able to apprentice newcomers if they chose.
Patients win, by regaining their clinician’s loyalty. Accountability improves in two ways. Responsibility for unlicensed employees rests directly upon the employer and/or supervisor. Unlicensed service providers are clearly private individuals, able to show proof of education or training, but operating without sanction of the state.
Taxpayers win by seeing more of their neighbors employed, and the state shed millions or even billions of dollars from its budget.
The next generation wins with more-accessible healthcare jobs.
Everyone wins with lower healthcare costs and more efficiency.
Objections
How does this work with non-professional healthcare workers?
Medicaid and other insurance billing demands are the primary reason for licensing non-professionals, who would otherwise work as employees or independent contractors. The solution is to channel Medicaid dollars through patients instead of plans, for example with Medicaid HSAs.
What about standards of care?
Standards of care are defined by those who give the care, and those who teach them. Professionals initially learn skills and relevant standards from an accredited educational program. As practitioners they continue to learn from peers, patients, and trusted resources.
Occupations and professions both come down to expertise learned on the job and in accredited educational programs. In both cases, educational certificates or diplomas serve as proof of qualifications, if needed.
What about legal liability?
If state credentials are no more than a barrier to lawsuits, they ought to be eliminated for that reason alone. Open communication, excellent care, and good patient relationships are the best protection from lawsuits.