- TriHealth names chief people officer
- Why hospitals should step away from data as the deliverable, per 1 exec
- State orders NYU Langone to restore gender care for youth
- San Diego provider opens 32-bed residential mental health facility
- Google’s pay for 3 health tech jobs
- Nevada hospital to downsize, switch to rural emergency status
- Nevada hospital to downsize, switch to rural emergency status
- Missouri system taps chief medical officer
- Moody’s downgrades Arkansas system’s credit rating
- Moody’s downgrades Arkansas system’s credit rating
- Mental health providers subject to ban on youth ‘transition’ procedures: Texas attorney general
- Epic, Oracle submit AI policy recommendations to HHS
- 5 gastroenterologist moves in 1 month
- Cost Plus Drugs partners to give hospitals easier access
- What’s new with Kaiser Permanente?
- 4 hospital, health system layoffs in February
- U of Mississippi pharmacy program targets maternal health crisis
- Innovate 32 continues growth, adds 2 dental practices in Tennessee
- Indiana hospital transitions revenue cycle operations to Revology
- New York surgery center inks anesthesia deal
- Mayo Clinic posts 6.8% margin in 2025
- 5 anesthesiologists in the headlines
- Listen to the Latest ‘KFF Health News Minute’
- Corewell Health posts 1.6% operating margin, grows revenue to $17.6B — 7 things to know
- Woodside Health acquires Arizona facility
- New York physician sentenced to 7 years for unlawful drug distribution
- Hasta los pacientes se sorprenden por los precios que sus aseguradoras están dispuestas a pagar, un costo que al final pagamos todos
- How to Get Ready For Daylight Saving Time
- A-Fib Drug Could Interact With Blood Thinners, Increase Risk Of Dangerous Bleeding
- Collagen Supplements Good For Skin, Arthritis, Evidence Review Concludes
- Effective Sunscreen Protection Can Cost $40 A Year
- Illicit Adderall Use Places Stress On The Heart, Study Shows
- Breast Cancer Cases, Deaths Expected To Rise Worldwide
- Readers Lean On Congress To Solve Crises in Research and Rehab
- Even Patients Are Shocked by the Prices Their Insurers Will Pay — And It Costs All of Us
- Federal Aid for Lead Cleanup Is Receding. That’s a Problem for Cash-Strapped Cities.
- Disc lays off 20% of employees to steady ship after FDA rejection of rare disease drug
- Novo plugs $500M into Ireland plant to produce Wegovy pill for markets outside US
- Esperion pays $75M-plus to acquire Corstasis and newly approved Enbumyst
- The dental workforce trends that will dominate 2026
- Federal Medicaid cuts threaten dental care access: See the potential impact by state
- Children’s Mercy raises $150M for mental healthcare
- California awards $291M to expand behavioral health housing, services
- OhioHealth builds well-being programs to reshape caregiver culture
- UF Health taps new outpatient senior VP
- UAMS names new director of cardiovascular medicine division
- CMS’ add-on billing code boosts specialist pay: Study
- Lawmakers introduce bill to reverse Medicaid cuts, expand Medicare benefits
- New Jersey woman charged with practicing unlicensed dentistry
- 100+ organizations call on CMS to revise 2027 MA rates
- Oklahoma advances interstate compact bill
- UNC Health Appalachian offers psychiatric physician training program
- Former PepperPointe Partnerships COO joins DPO
- The Smilist expands into Virginia
- Colorado Medicaid ABA audit finds $77.8M in improper payments
- Georgia opens 30-bed forensic mental health unit to ease jail backlog
- Pennsylvania county cuts ribbon on $19.8M mental health diversion center
- UHS to roll out behavioral health revenue cycle AI tools in 2026
- UHS to roll out behavioral health revenue cycle AI tools in 2026
- In 1 state, large hospitals dominate 340B's net savings
- 15 dentists making headlines
- CMS to suspend enrollment into Elevance’s Medicare Advantage plans
- Report: Most states investing in value-based care with Rural Health Transformation Program
- U.S. Tops 1,100 Measles Cases This Year as Outbreaks Grow
- FDA To Offer Cash Bonuses for Faster Drug Reviews
- 10 providers seeking RCM talent
- PDS Health added de novos across 3 states in February
- 'One2PrEP': Gilead's 1st Yeztugo DTC ad reimagines hit song to highlight biannual dosing
- GLP-1s support heart attack recovery in rodents by relaxing tight blood vessels
- Former Optum CEO Heather Cianfrocco to depart UnitedHealth Group
- New Drug, Acoziborole, Could Boost Efforts to Wipe Out Sleeping Sickness
- Chocolate Male Supplement Recalled Over Hidden Erectile Dysfunction Drug
- Amid unfolding Middle East war, pharma giants keep close eye on employee safety, supply chains
- CMS set to suspend enrollment in Elevance Health's Medicare Advantage plans
- Providers urge Education Department to reconsider which jobs face stiffer student loan caps
- Kennedy adds 2 new members to CDC’s vaccine panel ahead of delayed meeting
- Kennedy adds 2 new members to CDC’s vaccine panel ahead of delayed meeting
- Urban Traffic Noise Disrupts Sleep, Affects Heart Health After One Night
- Hormone Therapy Might Be Unnecessary For Some Prostate Cancer Patients
- Benzodiazepine Use Down In U.S., But OD Risk Remains, Study Says
- GLP-1 Drugs Might Ease Chronic Migraine, Study Says
- Blood Test Reveals Alcohol-Related Liver Disease
- Telemedicine Visits Cost Five Times Less Than In-Clinic Care
- Families Defend Disability Services Amid Medicaid Cuts
- Medicaid Is Paying for More Dental Care. GOP Cuts Threaten To Reverse the Trend.
- Bavarian Nordic CEO to follow board chair out the door after failed private equity takeover
- Ascendis gains more altitude with FDA approval for dwarfism drug Yuviwel
- CDMO Quotient extends Ipsen supply pact for rare disease drug Sohonos
- Quest Diagnostics launches Google-powered AI chatbot to help patients understand lab results
- Tennr takes aim at phone call bottlenecks as it builds out automation for patient referral process
- DoseSpot, Arrive Health merge to combine prescribing tools with pharmacy, medical benefit data
- Why Digital Tool are Needed to Cope with Increasing Pressures in MedTech Innovation
- Why Digital Tool are Needed to Cope with Increasing Pressures in MedTech Innovation
- Electronics Pollution Pose Added Threat to Endangered Dolphins, Porpoises
- Flea And Tick Pills May Pose Environmental Risks, Study Finds
- ICE, ALS, Addiction Medicine, and Robotic Ultrasounds: Journalists Sound Off on All That and More
- Iowa dentist surrenders license
- A Canadian Hospital Scoops Up Nurses Who No Longer Feel Safe in Trump’s America
- Statement on the Adoption of Final Rules Under the Holding Foreign Insiders Accountable Act
- Statement on Final Rules for the Holding Foreign Insiders Accountable Act
- State Medicaid budgets to weather $664B reduction through 2034 due to OBBBA: RAND
- Clover Health CEO said company sees opportunity in complex MA environment
- How pharma marketers are capturing the power of podcasts to connect with consumers
- Cigna's Evernorth quietly acquires hospital pharmacy CarepathRx
- Walgreens debuts virtual weight management clinic with access to GLP-1 meds
- New Obamacare Rules Could Raise Deductibles to $31K For Families
- Study Suggests One Common Amino Acid May Affect How Long Men Live
- Merck to wind down Gardasil production at N.C. plant, lay off 150-plus
- Walmart Great Value Cottage Cheese Recalled Over Pasteurization Issue
- Chris Bosh Says He’s 'Lucky To Be Alive' After Sudden Health Scare
- Patrick Kennedy: Collab with MAHA is essential to address mental health crisis
- Lilly debuts Nvidia supercomputer with fanfare and focus on escaping traditional pharma lifecycle
- Alignment CEO John Kao offers measured response to proposed 2027 MA rates
- Sanofi, Genentech, Kedrion back star-studded bleeding disorder awareness campaign
- Op-ed: Our patients deserve better safety reporting. AI could be the answer
- After CHMP nod, Moderna CEO applauds EU's 'rigorous scientific review'
- UCB's fast-growing Bimzelx leaps across blockbuster sales threshold as HS momentum builds
- Blood Test Can Predict Short-Term Survival Among Seniors
- How the Brain Learns to Have Seizures During Sleep
- Why Turning 19 Spikes Medicaid Loss for Millions
- Crash Course Might Speed Brain Stimulation Treatment For Depression, Study Suggests
- Wildfire Smoke Linked To Increase In Violent Assaults
- More Parents Are Refusing A Life-Saving Shot For Their Newborns, Study Finds
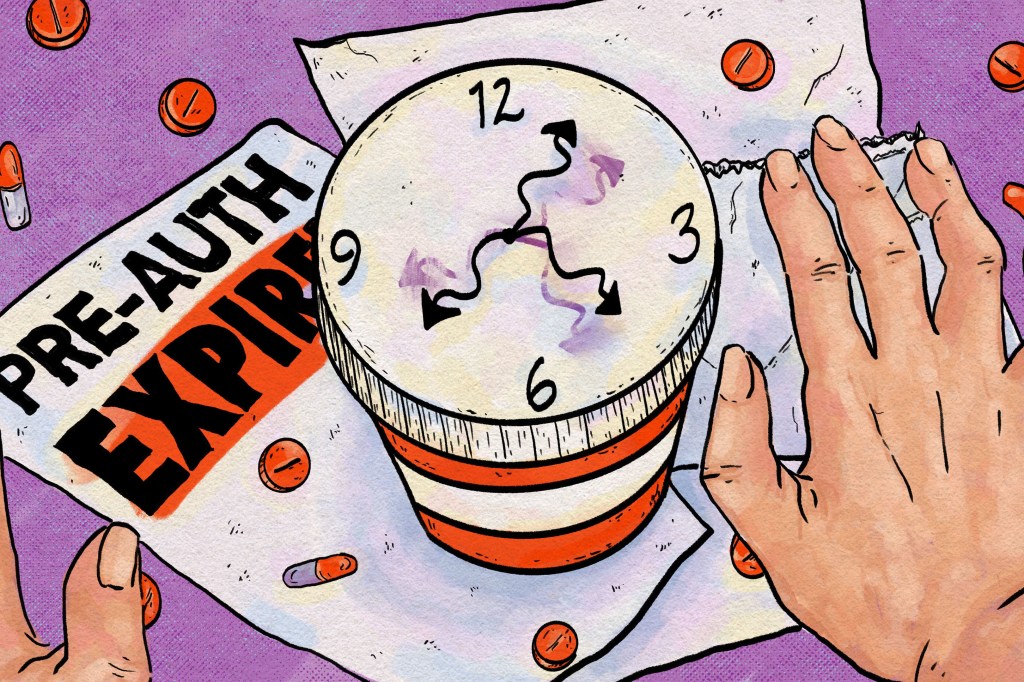
- To Avoid Care Disruptions, Know When the Clock Runs Out on Your Prior Authorization
- As SCOTUS takes on 'skinny label' review, top US lawyer sides with generics maker
- Lake Nona Impact Forum: There can't be longevity without tech
- FDA Approval for BIOTRONIK Solia CSP S Pacing Lead For LBBAP
- FDA Approval for BIOTRONIK Solia CSP S Pacing Lead For LBBAP
- Catalyst OrthoScience gets FDA 510(k) Clearance of Archer® Patient-Specific Instrumentation for Shoulder Arthroplasty
- Catalyst OrthoScience gets FDA 510(k) Clearance of Archer® Patient-Specific Instrumentation for Shoulder Arthroplasty
- Smith+Nephew signs distribution agreement with SI-BONE
- Smith+Nephew signs distribution agreement with SI-BONE
- Quantum Surgical Acquires NeuWave Medical, Inc.
- Quantum Surgical Acquires NeuWave Medical, Inc.
- How Pharma is Expanding its Global Footprint to Advance Clinical Research
- Partnering to Advance Drug Delivery Innovation
- Teladoc Health reports slower growth, offers cautious 2026 outlook as it shifts telehealth model
- CFO Mark Kaye to take the helm at Carelon in leadership shake-up at Elevance Health
- Insurance groups say proposed flat Medicare Advantage rates fail to meet the moment
- Health Gorilla urges court to toss lawsuit filed by Epic, health systems
- Stryker launches Synchfix™ EVT, expanding options for flexible syndesmotic fixation
- Stryker launches Synchfix™ EVT, expanding options for flexible syndesmotic fixation
- Democrat-Led States Sue Trump Administration Over Cuts to Childhood Vaccine Schedule
- CDC Vaccine Advisory Panel To Revisit COVID Shot Safety Next Month
- Frozen Blueberry Recall Issued Across Four States for Listeria
- After delay, CDC vaccine panel sets new dates to discuss long COVID and mRNA shot safety
- Decision Criteria for Technology Commercialization of Medical Devices in 2026
- Decision Criteria for Technology Commercialization of Medical Devices in 2026
- Continuous Cardiac Monitoring: Redefining the “End” of a Clinical Study?
- Continuous Cardiac Monitoring: Redefining the “End” of a Clinical Study?

In the pharmaceutical world, PBMs are the connected, protected middlemen.
The top three PBMs each excluded roughly 600 drugs from their 2023 formularies.By Maia Anderson April 4, 2023 · 5 min read
Pharmacy benefit managers (PBMs) are leaving more drugs off their formularies, which may prompt doctors to prescribe drugs that aren’t as effective or are more costly.
PBMs are companies that work on behalf of insurers and negotiate with drug manufacturers to create formularies, which are lists of drugs the insurers cover. PBMs also create lists of the drugs they exclude from their formularies, and these drugs therefore don’t get covered.
When drugs are left off formularies, patients have to pay more out of pocket to get the drugs they need. For those who can’t afford it, that can mean worse health outcomes and higher overall healthcare costs.
Exclusion lists have gotten longer every year, and these most often affect drugs for chronic illnesses, according to research from Xcenda, a pharmaceutical consulting firm owned by drug wholesaler AmerisourceBergen (which is expected to rebrand as Cencora in 2023).
“Who bears the consequences is really the prescriber, from a liability standpoint and also from a patient care standpoint. The patient can potentially have poor outcomes,” Robert Popovian, chief science policy officer at the Global Healthy Living Foundation, a nonprofit that advocates for increased access to healthcare services for people with chronic illnesses, told Healthcare Brew.
Back in the day
Formularies were initially created to make sure doctors prescribed patients the least expensive drugs that were still effective, according to research that Popovian conducted with the foundation in 2022.
PBMs began making formulary exclusion lists in 2011, according to Xcenda. CVS Caremark was the first to do so for the 2012 plan year, followed by Express Scripts in 2014 and Optum Rx in 2016.
Since then, the number of drugs left off formularies has risen sharply. In 2014, at least one of the top three PBMs excluded a total of 109 drugs, and in 2022, that number rose to 1,156, according to Xcenda’s research. In 2023, the top three PBMs each excluded about 600 drugs from their formularies, according to Drug Channels data.
There’s no legal limit to how many drugs PBMs can exclude, said Popovian.
Of the 1,156 drugs left off formularies in 2022, nearly half were brand-name medications that didn’t have a generic equivalent, according to Xcenda.
Leaving out chronic conditions
Drugs that treat chronic conditions such as diabetes, cardiovascular disease, dermatological conditions, and central nervous system disorders are most frequently affected by PBM formulary exclusions, according to Xcenda’s research.
Cancer drugs are also increasingly left off formularies, Xcenda’s research found. Express Scripts left 46 cancer drugs off its formulary between 2014 and 2022, accounting for 7% of its exclusions, the firm reported. CVS Caremark excluded 32 cancer drugs during the same time period, and Optum Rx excluded 30.
Drugs approved via one of the FDA’s four expedited approval pathways, including the accelerated approval pathway, are left off formularies more often, Xcenda’s research found. The pathways are designed to speed up the approval process for drugs that treat serious conditions. Between 2014 and 2022, PBMs excluded 178 drugs approved through one of the pathways for at least one year.
“The ultimate consequences for patients when they don’t get access to the drug that’s appropriate for them is obviously mortality or morbidity. Unfortunately, PBMs don’t want to take responsibility for that,” said Popovian.
PBMs do offer a pathway for patients to apply and get coverage of a drug on the exclusions list, but the process “can be time-consuming and burdensome for both the patient and their physician,” according to Xcenda.
“In my opinion, the solution is to go back to a tiered formulary where you have reasonable out-of-pocket costs for patients, and the patient and the prescriber—the clinician—can decide what is best for them, and they have access to all of them,” Popovian said.
An expensive swap
PBMs usually argue that the drugs they exclude generally have alternatives that are as equally as safe and effective, said Popovian. But according to his research, nearly half of all drug exclusions require doctors to prescribe medications that may have “adverse financial or medical outcomes for their patients.”
They also sometimes replace cheaper drugs with more expensive ones. In an analysis of Express Scripts’s 2022 formulary exclusions list, Popovian found that in 10 cases, the PBM excluded generic drugs in favor of “significantly more expensive” brand-name drugs. In some cases, the PBM excluded drugs from coverage without providing any alternatives.
“Although some formulary exclusions may be clinically and economically justified, a significant number require healthcare professionals to make medical decisions that may not be in the patient’s best interest or aligned to current standards of care,” Popovian wrote in the study.
CVS Caremark declined to comment. Optum Rx and Express Scripts did not respond to Healthcare Brew’s requests for comment.
Maia is a Los Angeles-based reporter for Healthcare Brew, where she specializes in coverage of the pharmacy industry. She has three years of professional journalism experience, and previously worked as a fellow covering the aerospace industry at Insider, as well as a healthcare reporter for Becker's Hospital Review. She has won an award from the Society of Professional Journalists for her work.
Hospital transparency is important, but the really juicy points here are about PBMs.
At a guess, the large body of misinformation about PBMs qualifies it for the Top 5 Lies of healthcare politics. Hard enough to understand where they come from (a few lies) and what they do (more lies) but then there's the real question - Do they save consumer costs? (lots of lies)
It's important to understand that not all PBMs are the same, and their lobbies reflect that here. Bold emphasis added to the "aha" points.
More Transparency Needed in Healthcare, House Members Told
— Lack of data from hospitals, PBMs in the spotlight at hearing
The U.S. healthcare system would be greatly improved by more transparency from all players, including hospitals, pharmacy benefit managers (PBMs), and insurers, members of Congress and witnesses agreed Wednesday at a House hearing.
"For too long medical prices have been shrouded in mystery and patients have lived in fear of how much their medical bills will end up costing them," Rep. Bob Good (R-Va.), chair of the House Education & Workforce Subcommittee on Health, Employment, Labor, and Pensions, said at a hearing on competition and transparency in healthcare. "The Trump administration issued a rule to require hospitals to give employers and consumers accurate pricing data. Hospitals were required to file this information, but only 25% of hospitals fully comply."
"We must push for standardized data and make it usable so employers can effectively meet their fiduciary obligations," he continued. In addition, "Congress must codify the transparency and coverage rule to ensure the administration enforces requirements that plans submit drug pricing data. Without this critical information, employers and patients will be left in the dark when it comes to navigating the complexities and costs of the drug supply chain."
Rep. Mark DeSaulnier (D-Calif.), the committee's ranking member, said he was interested in changing the incentives of PBMs to make sure they act in the best interest of clients. "At a minimum, we should all agree that employers and consumers deserve to know how the rebates PBMs receive from drug manufacturers impact their decisions that raise costs for workers and families."
Gloria Sachdev, PharmD, president and CEO of the Employers' Forum of Indiana, a coalition of employers interested in healthcare affordability, expressed frustration about PBM transparency. "None of our employers have seen any pharmaceutical claims data at the drug level," she said. "When they get rebate information, they get it in aggregate. So that's not helpful to the employer because then they can't shop for it."
"They are told, 'If you want to change the formulary, then that might impact the rebates that we give you.' Let's say they have 500 drugs that they're covering, maybe more, and we would want to see what the rebates are at the drug level. We don't get that level of information at the drug level," she added.
Sachdev noted that the Indiana state legislature recently addressed the hospital pricing issue, passing a law that barred hospitals from billing additional hospital facility fees for off-campus services. "Just because a hospital buys a physician clinic in a strip mall does not mean they should be allowed to add on hospital facility fees when nothing about the service or doctor or location has changed," she said. "Tacking on hospital facility fees can easily double the price for no reason. We should pay the same amount for the same service regardless of who owns it."
The hearing also featured two very different witnesses from the PBM industry. J.C. Scott, president and CEO of the Pharmaceutical Care Management Association (PCMA), which represents large PBMs including CVS Health, Express Scripts, and Optum Rx, said that "efforts to lower drug costs must start with an understanding that drug prices are set by drug companies and that in the prescription drug market, as in many markets, competition is vitally important."
"Lawmakers must ensure that the misuse of the patent protections originally put in place to balance rewarding innovation and ensuring affordable access for patients is not blocking competition and keeping prices high," he noted.
Greg Baker, CEO of AffirmedRx, a PBM based in Louisville, Kentucky, said his company doesn't belong to PCMA because "PCMA does not represent who we are as an organization. We have founded a new not-for-profit organization with numerous other PBMs who also do not want to be represented by PCMA, called TransparentRx."
"I would like to embrace many of the much-needed reforms gaining steam in Congress," he said. "PBMs, especially traditional ones, and especially the big three, deserve scrutiny and reform. More importantly in my opinion, their approach is a central feature to sustaining unnecessarily high drug costs in America. We have a broken system which hides profits and inflates prescription costs, harming the interest of diverse communities, working families, and seniors."
The idea that PBMs promote generic drug use "is a falsehood," Baker said. "You can look at any traditional PBM formulary that's publicly available online and consistently see where brand-name drugs are put in place on the formulary over generic drugs. And when you consider the fact that of the 160-[million]-plus Americans who take private insurance, that 55% of those people have a coinsurance or a high deductible plan, that means they are subject to a higher cost at the pharmacy counter. That is not acceptable in our opinion."
Rep. Pramila Jayapal (D-Wash.) wanted to talk about hospital consolidation. "We've seen a concerning increase of [hospital] mergers across the country," she said. "A recent report by The New York Times found that areas with the highest rates of hospital consolidation had prices go up between 11% and 54%."
The hospital business model has undergone a big shift, said Sophia Tripoli, MPH, director of healthcare innovation at the consumer group Families USA. "It's based on two things: buying up local competition to gain more negotiating leverage over how to demand higher prices, and generating high volumes of high-priced services," she said. "And the results of course [are that] the prices get passed on -- particularly in the commercial market -- to employers. We see stagnant wages, we see increased premiums and cost-sharing for consumers, and we're stuck with unaffordable healthcare."
https://www.medpagetoday.com/publichealthpolicy/healthpolicy/105122
An inside view of PBMs: MedPage Today features this op-ed from a breast cancer specialist.
https://www.medpagetoday.com/opinion/second-opinions/105764
In a Golden Age of Cancer Care, PBMs Are Holding Us Back
— We must stop predatory and destructive behaviors
We're living in a remarkable time for cancer treatment, when a diagnosis no longer disrupts how patients live and work. Unlike years ago, an advanced cancer diagnosis is no longer a death sentence for many. Today, most patients diagnosed with cancer can treat it as a chronic disease, much like hypertension and diabetes. Patients undergoing cancer treatment can go to work, pick their children up from soccer practice, and eat dinner with their families.
This is largely due to oral cancer drugs, which allow many cancer patients to maintain a normal routine and quality of life. These treatments are rapidly on the rise: today, oral cancer drugs account for25-35% of cancer therapiesin development, a number that is projected to grow to 60% in the next few years.
As pharmacy benefit managers (PBMs) have become vertically integrated -- with just three organizationsdominating 80%of the prescription drug marketplace -- cancer patients receiving oral treatment are increasingly forced to endure PBMs' excessive approval processes and are directed to PBM-owned mail order or specialty pharmacies that refill drugs. These companies, many of whom are owned by or own the largest health insurers, want to control what treatment patients get and how, when, and where they receive it.
As a breast cancer specialist, I've witnessed how these middlemen insert themselves between patients and doctors through an opaque system of authorizations, barriers, and fees that delay patients' access to life-saving treatment.
Last October, I saw my patient Tania*, a 40-year-old woman with metastatic breast cancer that had metastasized to her brain. I recommended that we utilize the oral cancer drug abemaciclib (Verzenio) due to its unique ability to help treat brain metastasis, which many cancer therapies do not treat. After going through her insurance company and PBM for authorization, the pills were denied. I quickly appealed, but the PBM informed us it would take 6 weeks just to be granted a peer review.
During this time, I watched as Tania's cancer continued to metastasize, and she was soon forced to resort to traditional chemotherapy -- a less effective, higher-toxicity treatment plan. Tania had to stop working and even developed two new brain metastases. While I don't know for certain that Tania would have been better off with abemaciclib,peer-reviewed literaturedemonstrates that she would have doubled her chances of living without cancer progression and would have experienced less toxicity in comparison with traditional chemotherapy.
My experience with Tania underscores a harsh reality: rather than assist in cancer care coordination, PBMs often cause disjointed, delayed, confusing, and inferior care.
That was just one frustrating example. Let's examine another.
Doctors frequently modify treatment doses to optimize therapy and control toxicity, sometimes just 1 to 2 weeks after starting treatment. These types of unplanned adjustments are easy to navigate in office-based, medically-integrated pharmacies that serve as a "one-stop shop" for oral cancer therapies, as oncologists can evaluate the patient, check their labs, and make dose modifications prior to the refill.
Yet, PBMs often use their ever-increasing market size and power todivert cancer drugsaway from physician dispensing pharmacies. The result is that patients are steered away from the dispensing pharmacy at their community oncology clinic and forced to use PBM-mandated specialty or mail order pharmacies; this may result in delays in prescription delivery, mix-ups, and bureaucratic red tape throughout. By virtually eliminating competition from physician dispensing, PBMs are capturing the prescription drug market -- with seemingly little regard for patient care.
PBMs may tell us that this bureaucratic arrangement is a cost-saving measure. Yet, we see no evidence that PBM involvement translates to patient or employer savings. In fact, premiums and out-of-pocket costs continue to rise. The average premium for family coverage in an employer-sponsored plan hasincreased 47%over the past decade, while patients' out-of-pocket spending on prescription drugsclimbedfrom 23.8% in 2013 to 25.1% in 2019 (spending fell in 2020, but this was likely due to the pandemic). Further, these abusive practices are used to allow PBMs to control the practice of medicine by removing treatment decisions from providers' hands.
Thankfully, bipartisan congressional efforts are shining the light of transparency on PBM behavior. In fact, PBM reform is so popular that Sen. Bill Cassidy, MD (R.-La.) and Sen. Bernie Sanders (I.-Vt.) -- ideological opposites on many issues -- are working across the aisle to pass thePharmacy Benefit Manager Reform Act(S. 1339), which would ban PBMs' use of certain predatory tactics, including spread pricing and claw back fees. With widespread bipartisan support, now is the time to add more oversight and transparency to these middlemen.
Cancer and other diseases know no political divide. It's long past time that we stop PBMs' destructive behaviors to ensure patients can fully realize the benefits of modern cancer therapies.
Debra Patt, MD, PhD, MBA, is an oncologist specializing in breast cancer in Austin, Texas. She serves in the leadership of Texas Oncology, a large independent community oncology practice that is part of the US Oncology Network, and as vice president of the Community Oncology Alliance.
Are PBMs the real problem? Or is it their cozy relationship with insurance companies and coverage determinations?
Get MHF Insights
News and tips for your healthcare freedom.
We never spam you. One-step unsubscribe.