- FDA vaccine chief to step down in April
- FDA, states collaborate to lower drug prices
- 84% of primary care providers say they have key role in mental healthcare: Survey
- 84% of primary care providers say they have key role in mental healthcare: Survey
- SAMHSA offers $69.1M in behavioral health grants
- California to invest $65M in new mental health, housing community
- Florida hospital selects new EHR
- New Mexico governor signs sweeping healthcare reforms: 5 things to know
- Kettering Health faces 44 lawsuits over cyberattack
- 10 hospitals, health systems looking for CFOs
- 10 hospitals, health systems looking for CFOs
- Highmark Health generates $28M in value with Google AI
- Hiring red flags for dental employers to watch out for
- 4 health systems with boosted outlooks
- 4 health systems with boosted outlooks
- Alabama dentist sentenced to 15 years in prison for arson, insurance fraud
- We turned off the phones and our practice got busier
- Allina physicians, NPs, PAs back open-ended strike
- ‘This is how we know if we’re winning or losing’: Inside Grand Mental Health’s KPI strategy
- The cardiology physician shortage by state by 2036
- How dentists can keep up with rising patient expectations
- New leadership appointments across 5 specialties
- Among pregnant ED patients, Tylenol use fell 10% after Trump linked drug to autism risk
- Henry Schein opens integrated dental-medical training facility
- Henry Schein opens medical-dental integrated ASC
- Why Behavioral Health Needs an Operating System, Not Another Point Solution
- What’s the status of the federal noncompete ban? 5 notes
- North Carolina appeals court rejects AdventHealth CON complaint
- Telehealth growth hasn’t increased rural behavioral healthcare access: Study
- The NIH Workforce Is Its Smallest in Decades. Here’s the Work Left Behind.
- 16 hospitals closing departments or ending services
- Texas dental school to launch oral surgery residency program
- Trump administration weighs looser policies on nursing home antipsychotic use
- 62 ophthalmology departments ranked by NIH funding
- California oral surgery practice suffers data breach
- Private equity’s big-money deals are back: 5 trends for ASCs and physicians
- Virginia board denies dentist’s license reinstatement request
- Bill to reauthorize funding for CDC’s oral health program introduced: 5 things to know
- Trial compares genetic risk-sharing methods for colorectal cancer
- UPMC acquires Pennsylvania GI practice
- North Carolina launches mobile crisis dispatch pilot
- HCA New Hampshire hospital to end outpatient mental health services
- HCA New Hampshire hospital to end outpatient mental health services
- Ohio dental board revokes dentist’s anesthesia permit, suspends license
- Virginia dental practice reopens after fire
- BCBS Michigan updates, clarifies policy set to cut 50% from some E/M payments with ‘modifier 25’
- KFF: A look at Part D enrollment trends for 2026
- Lonza hands off capsule business to investment firm Lone Star in $3B deal
- Fitch downgrades Michigan hospital’s credit rating
- Some Patients Keep Weight off With Fewer GLP-1 Injections, Study Finds
- Christus Health doubles operating income in H1
- Democrats press 11 pharmas for 'any evidence' their Trump pricing deals deliver savings for Medicaid
- Democrats press 11 pharmas for 'any evidence' their Trump pricing deals deliver savings for Medicaid
- RFK Jr. Urges Medical Schools To Add More Nutrition Training
- Sixth Measles Case Confirmed in New Mexico Jail
- Sanofi strikes deal with Brazil's EMS to sell generics manufacturer Medley
- Philips unveils Rembra CT for acute and high-demand imaging environments
- Philips unveils Rembra CT for acute and high-demand imaging environments
- 45,000 Halo Magic Sleepsuits For Babies Recalled Over Choking Risk
- Super Bowl, Winter Olympics defined TV drug ad spending in February, led by AbbVie’s Rinvoq
- Op-Ed—American healthcare has a pricing problem
- Taiwan earmarks $755M for multi-year drug supply resilience program
- GLP-1 Weight-Loss Drugs Prove Effective Across Diverse Patient Groups
- Angry Teens May Age Faster, Study Finds
- Chronic Pain Can Make Noise Unbearable By Rewiring The Brain, Study Says
- Telemedicine Not Closing the Mental Health Gap in Rural Areas
- Racial Disparities Persist In Lung Cancer Treatment, Study Finds
- Peanut Allergy Risk Higher If Older Sibs Eat Peanuts, Study Finds
- FDA to end 9-month advisory committee drought with April review of AstraZeneca’s oral SERD, Truqap
- Pfizer breaks into obesity market in China with approval for Sciwind-partnered GLP-1
- This Doctor-Senator Who Backed RFK Jr. Now Faces a Fight for His Job — And His Legacy
- The People — And Research — Lost in the NIH Exodus
- Six Federal Scientists Run Out by Trump Talk About the Work Left Undone
- Servier to widen rare cancer offerings with $2.5B buyout of Day One and glioma drug Ojemda
- Fierce Pharma Asia—Kyowa ends OX40 program; Sanofi licenses first-in-class drug; BioNTech advances Duality ADC
- 47,000 comments on MA payment rule for 2027 breaks CMS record
- ‘Calm urgency’: How 1 Louisiana CFO tackles transportation, payer pressure and margins
- Moody’s downgrades Children’s Hospital of Los Angeles’ credit rating
- What the Health? From KFF Health News: 40 Years of Health Policy
- Salesforce partners with HealthEx, Verily and Viz.ai to build out healthcare AI agents
- J&J's Tecvayli-Darzalex multiple myeloma combo takes home FDA's 3rd national priority nod
- Rising Tree Pollen Counts Signal Start of Allergy Season
- Experts call for more data, collaboration to address gun violence at annual Northwell forum
- Finding the Right Supportive Footwear for Pain Relief is Key, Say Podiatrists
- FTC seeing 'progress' in discussions with Optum, Caremark in insulin case
- Fewer Mothers Died During Pregnancy or After Birth in 2024
- Trader Joe's Pulls Frozen Meals Tied to 37 Million-Pound Nationwide Recall
- Optum teams with Microsoft to expand AI-powered claims platform
- RadNet Acquires Gleamer to Support Position as a Radiology Clinical AI Solutions Leader
- RadNet Acquires Gleamer to Support Position as a Radiology Clinical AI Solutions Leader
- Study: PE's primary care purchases add clinicians, but also increase turnover
- Ultrasound AI Receives FDA De Novo Clearance for Delivery Date AI Technology
- Ultrasound AI Receives FDA De Novo Clearance for Delivery Date AI Technology
- Abbott CardioMEMS™ remote heart failure monitoring reader receives FDA approval
- Abbott CardioMEMS™ remote heart failure monitoring reader receives FDA approval
- As AI evolves, the modern R&D lab is changing
- Dozens of medical schools meet RFK Jr.'s call for greater nutrition education
- BD Gets CE Mark for Revello Vascular Covered Stent
- BD Gets CE Mark for Revello Vascular Covered Stent
- FDA gives Glenmark thumbs up for first 'true' generic version of GSK's asthma inhaler Flovent
- After generic defense fails, Merck KGaA assumes no US Mavenclad sales after March
- Fitness Trackers Might Help Predict Multiple Sclerosis Progression
- Dentists Can Help Detect Undiagnosed Diabetes, Study Argues
- Half of Americans Unaware of At-Home Colon Cancer Screening Options
- Ultra-Processed Foods Linked To Emotional, Behavioral Problems In Preschoolers
- Study Links Rising Cannabis Use to Poor Mental Health
- Testosterone Therapy Could Mean Trouble For Knee Replacement Patients, Study Warns
- Galderma doubles Nemluvio peak sales projection to $4B-plus after strong atopic dermatitis launch year
- Leo roars onto Netflix with DTC campaign for new hand eczema cream Anzupgo
- Con la presencia del ICE, habitantes de Minnesota crearon un sistema médico en las sombras. Un aprendizaje para otras ciudades
- Trump’s Cuts to Medicaid Threaten Services That Help Disabled People Live at Home
- Listen: What To Do When Health Insurance Slips Out of Reach
- As ICE Moved In, Minnesotans Set Up a Shadow Medical System. It’s a Lesson for Other Cities.
- Forma Life Sciences launches with oral solid dose focus, joining class of new CDMOs
- AWS offers agentic AI solution to tackle scheduling, ambient note-taking and medical coding
- Opening Remarks at Private Markets Roundtable
- Eli Lilly launches its direct-to-employer platform for obesity drugs
- Eli Lilly launches its direct-to-employer platform for obesity drugs
- Hospitals decry drugmakers' expanded claims reporting policies for 340B
- CVS unveils Health 100, its new Google-powered consumer engagement platform
- Remarks at Financial Stability Oversight Council Artificial Intelligence Innovation Series Roundtable on Strategy and Governance Principles
- Collegium enrolls Paris Hilton in Jornay PM push encouraging ADHD community to 'Embrace Your Sparkle'
- Review of U.S. Measles Elimination Status Delayed Until November
- Your Furry Roommate May Be Affecting The Air You Breathe
- BioDuro enters Taiwan joint venture, adding commercial API plant to production network
- FDA answers Vanda's yearslong call for public hearing on unsuccessful jet lag approval bid
- MUSC Health acquires South Carolina's largest multispecialty practice for $111M
- About 81,000 Baby Monitors Recalled Over Possible Fire Risk
- Armed with funding and an acquisition, Procode AI launches AI-powered RCM for surgical billing
- Charities merge to form nation's 'most comprehensive' patient assistance nonprofit
- Two Days of Oatmeal May Lower Cholesterol, Study Finds
- Bayer looking at another year of 'resilience' before growth kicks in behind Nubeqa, Kerendia
- Colorectal Cancer Rates Shifting to Younger Groups as Rectal Cancer Rates Spike
- Brain Chemical Provides A 'Pep In Your Step,' Experiment Shows
- Lithium Might Slow Brain Decline Among Seniors, Pilot Study Shows
- Exercise Boosts Quality of Life During Breast Cancer Chemotherapy
- Early Sports Specialization Linked To Increased Injury Risk
- More Kids, Teens Injured In E-Bike Wrecks, Study Finds
- Novo lands another FDA untitled letter, this time for Apple-inspired Ozempic ad
- Moderna fronts $950M to settle yearslong COVID patent litigation with Genevant, Arbutus
- Despite Their Successes, Some Mobile Crisis Response Teams Are in Crisis
- Healthcare’s mixed Q4, plus insights from the Lake Nona Impact Forum
- FDA ramps up crackdown on GLP-1 drug compounding with fresh batch of 30 warning letters
- HCA Healthcare says all-time high inpatient occupancy, ACA exchange attrition won't spoil 2026 volume growth
- Papa rolls out new program for insurers called Papa Plus
- AI Therapist? It Falls Short, a New Study Warns
- Grow Therapy scores $150M to build out enterprise partnerships with docs, employers
- Nearly 20 States Scale Back HIV Medication Programs
- BBQ Sauce Recall Issued Nationwide Due To Incorrect Label
- FDA Recalls More Than 651,000 Jugs of Water Over Sanitation Concerns

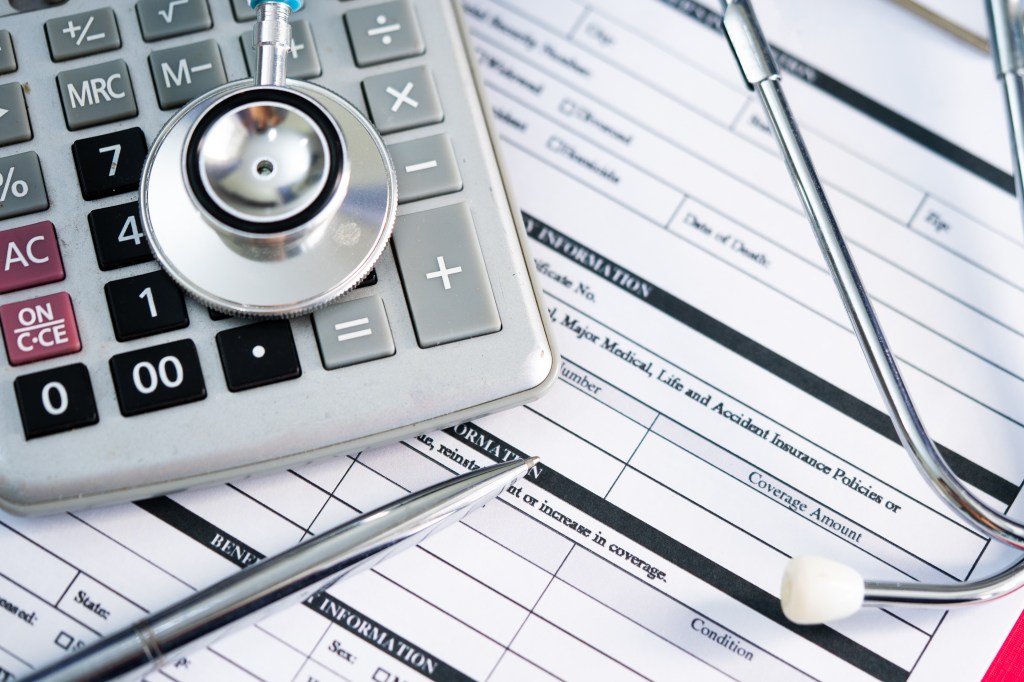
It should come as no surprise that PPACA health plan buyers traded down from the higher tier, more expensive plans to lower tier plans with higher deductibles for the 2026 plan year. This won't change, even if the Congress extends the pandemic super subsidies (and that is looking ever more unlikely). Any subsidy extension would have to allow reopening of PPACA health care plan choices to affect this trend:
More Americans are picking higher-deductible Obamacare plans, possibly risking their health
The loss of enhanced subsidies and premium sticker shock are driving the trend, state officials and policy experts say.
By Robert King - February 4, 2026More Americans are turning to cheaper Obamacare plans to avoid premium sticker shock, according to preliminary data from states.
But the switch comes with a caveat: thousands in extra out-of-pocket costs that policy researchers say may make people hesitate to get medical care when they are sick or injured.
“I think buying down this year is a reflection of affordability,” said Stacey Pogue, senior research fellow with Georgetown University’s McCourt School of Public Policy. “People who are doing it want to cling on to coverage.”
Rising consumer costs have become a pivotal issue in the battle for control of Congress in the midterm elections this fall, beginning when Democrats blamed Republicans for failing to agree on a plan to extend enhanced subsidies. The impasse triggered a record-length shutdown of the federal government last fall, further highlighting the issue.
Now Republicans and the White House are pushing for ways to address affordability across a range of categories, while Democrats are expected to make soaring premiums on the Affordable Care Act insurance exchanges a key plank of their campaign to retake Congress.
The subsidies’ expiration on Jan. 1 caused annual premiums to spike more than $1,000 on average for subsidized enrollees, according to one estimate from the health research organization KFF.
Signups for 2026 declined by 1.2 million — or five percent — to 22.9 million, compared to 24.1 million in 2025, according to a national enrollment snapshot released by the Centers for Medicare and Medicaid Services for 2026 Obamacare coverage.
The drop — which some experts are concerned will increase as the year unfolds — occurred primarily on the 30 state exchanges run by the federal government, totaling 9 percent. Several of the states running their own exchanges have seen increased enrollment, perhaps in part because they used their own money to compensate for the loss of subsidies for lower-income customers.
But even in those states, officials are noting a significant trend: More Americans are downgrading to so-called bronze tier plans that have lower premiums but higher deductibles — 40 percent higher, by about $2000, compared to the next highest silver tier plan, which offers coverage with a lower deductible and higher premiums.
California, for instance, saw its enrollment hold steady for 2026 with around 1.9 million people choosing coverage, just a 2 percent drop from last year.
However, both new and returning customers are overwhelmingly choosing lower-tier plans. In 2026, more than a third of new enrollees chose bronze plans, compared to less than a quarter last year. For people who stayed in the marketplace, but switched tier levels, 73 percent switched to a bronze plan, compared to 28 percent last year.
Maine also saw more consumers selecting bronze plans. Enrollment increased by more than 10 percentage points compared to the year before. Bronze plans now make up nearly 60 percent of all state plan selections, which include silver, gold and catastrophic plans, according to a press release from the state.
Rhode Island’s exchange saw a slight decrease in enrollment and an explosion of signups for bronze compared to 2025, according to state data shared with POLITICO.
The number of people who chose a bronze plan increased 140 percent, from 848 people for 2025 to 2,053 for 2026. Silver tier enrollments held steady, but gold and platinum tier plans — which have the highest premiums and lowest deductibles — saw declines of 16 percent and 18.6 percent, the state data shows.
CMS is likely to release more data on enrollment this summer, which will give more insight into how many Americans shifted into bronze or catastrophic plans.
What’s in the plan
Bronze plans must cover the same benefits as other plan tiers sold on the ACA’s insurance exchanges. The catch is they require patients to shoulder a greater amount of cost-sharing.
This year, the average bronze plan for an individual had a deductible of $7,476, about 40 percent more compared with $5,304 for a silver plan. In most instances, the full deductible must be paid before any co-pays go into effect.
Another option is catastrophic plans, which have even lower premiums but very high deductibles, averaging $10,600 for an individual and $21,200 for a family. However, these plans are not available in every state and can only be bought by people under 30 or those over 30 who have a hardship exemption.
Several experts say that Americans are making the switch to a lower-tier plan because it’s still better than nothing. But the calculation can come with costs for good health.
“If you have an expensive health care encounter or expensive illness, you will be responsible for paying that deductible entirely out of pocket,” said Emma Wager, senior policy analyst for the Affordable Care Act program for KFF.
Several studies have shown high-deductible plans can be a barrier to care. An April 2025 study published in the Journal of the American Medical Association of more than 300,000 adults showed people in high-deductible plans were less likely to use clinic, lab or prescription drug care across several chroniEc illnesses.
A 2023 study published in the journal Translational Behavioral Medicine analyzed the behavior of nearly 26,000 people with different insurance types. The group with high-deductible plans was less likely to visit physicians, get screenings or receive the flu vaccine, even though the latter two are usually free for preventative care.
Silver problems
There is a quandary for some low-income customers who may be stuck with higher premiums.
Low-income ACA customers who earn between 100 to 250 percent of the federal poverty level (or between $15,560 and $39,125 for an individual) can get a cost-sharing reduction that can dramatically lower their annual deductibles to as little as $80.
To receive a CSR, though, an ACA customer must buy a silver tier plan, even though the premiums are higher than they are for bronze plans. The average lowest cost bronze plan has a monthly premium of $456 compared with $611 for the average lowest silver tier plan. That cost can vary from state to state and could come down with the base ACA subsidy that remains intact.
Last year, roughly half — 53 percent — of all enrollees on the ACA marketplace got some form of CSR attached to silver plans, according to a KFF analysis.
Those individuals now have to weigh paying a much higher premium or risk the much higher bronze plan deductible.
HSA hurdles
Bronze and catastrophic plan holders are now eligible for a health savings account, which enables them to put tax-free money into an account that can be used for a variety of health needs. Those needs can include paying down deductibles, but they can not be used to help pay premiums.
However, an HSA is only as good as the amount of money devoted to it. Right now, bronze plan holders would have to contribute to their own HSAs — an unlikely scenario for people who have downgraded plans because of affordability.
Republicans have pushed for government-funded HSA accounts. One proposal from Sen. Bill Cassidy (R-La.) would convert enhanced subsidy funding into government-funded HSAs.
However, Democrats have been cool to such an approach. Congressional Republicans could decide to add the proposal in a party-line reconciliation bill, but have not finalized whether they will put such a megabill together yet this year.
The question of how many Americans move to bronze and catastrophic plans will continue to play out over the next few months, including what it means for the exchanges, which rely on a healthy population to help maintain the stability of the risk pools.
That stability could be upended if people drop out after using their health coverage and deciding a high deductible isn’t worth it.
“People who drop out are going to be the healthier people,”said Jason Levitis, senior fellow with the left-leaning think tank Urban Institute. “People who are sick and have large health expenses are going to have to find a way to pay their premiums. It is going to be bad for the market.”
States are also watching to see how many people pay their premiums this year or decide to drop out.
It could change the conversation about affordability on the exchanges, Pogue said.
“We saw a lot of attention on whether net premiums are going to be affordable, but moving forward there will be a lot of talk about whether people who cling to coverage are getting care available,” she said.
Get MHF Insights
News and tips for your healthcare freedom.
We never spam you. One-step unsubscribe.