This NIH racialist program grant may or may not be associated with the MDHHS Advancing Healthy Births plan:
https://obgyn.msu.edu/research/the-miracle-center
MATERNAL HEALTH MULTILEVEL INTERVENTIONS FOR RACIAL EQUITY (MIRACLE) CENTER
Reducing disparities in pregnancy-related illness and death among African American, Hispanic, and rural populations in Michigan.
The Center will be rooted in a culturally informed research community with longstanding involvement from community, health, and policy partners. Critically important partners will also include Black and Hispanic Medicaid-eligible mothers, parents, and their families.
Cris Meghea, Jennifer E. Johnson, and Peggy Vander Meulen lead the Center (U54HD113291). Supporting the Department, College, and University commitment to advance women’s health and health equity, this U54 Maternal Health Research Center of Excellence was funded to address maternal morbidity and mortality disparities across Michigan. It is one of 10 Centers of Excellence nationwide that NIH is funding through their IMPROVE (Implementing a Maternal health and PRegnancy Outcomes Vision for Everyone) initiative. The NIH funding amount for the Center is close to $19 mil. over 7 years starting in 2023.
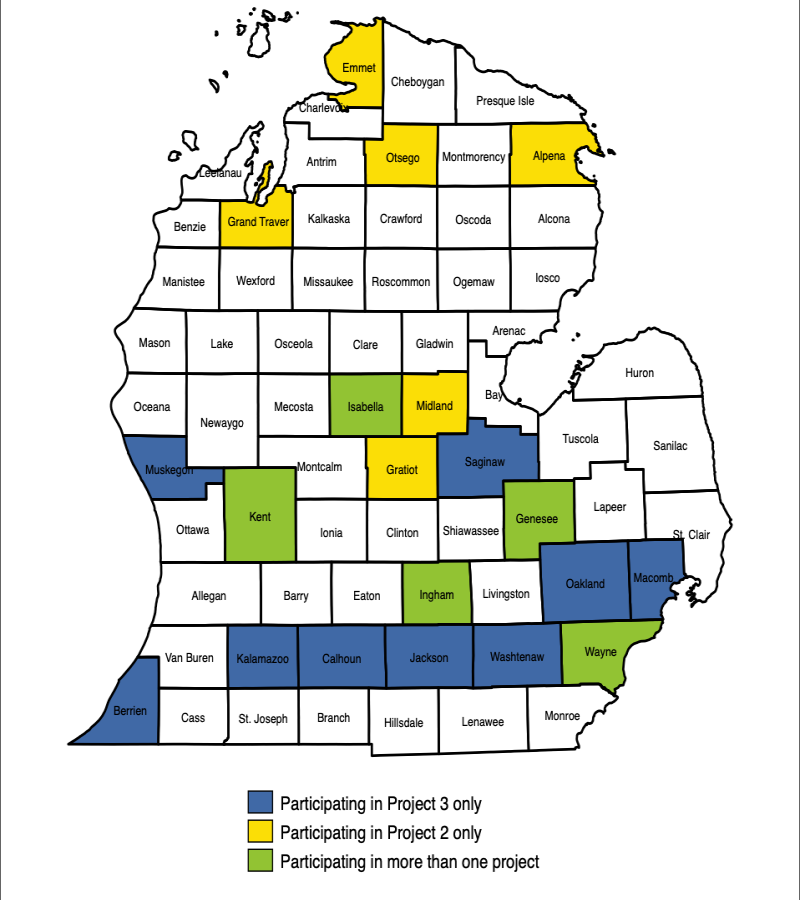
Birthing individuals and their families in 20 counties throughout Michigan will be impacted by the work of the Center, covering a population of more than 7 million individuals.
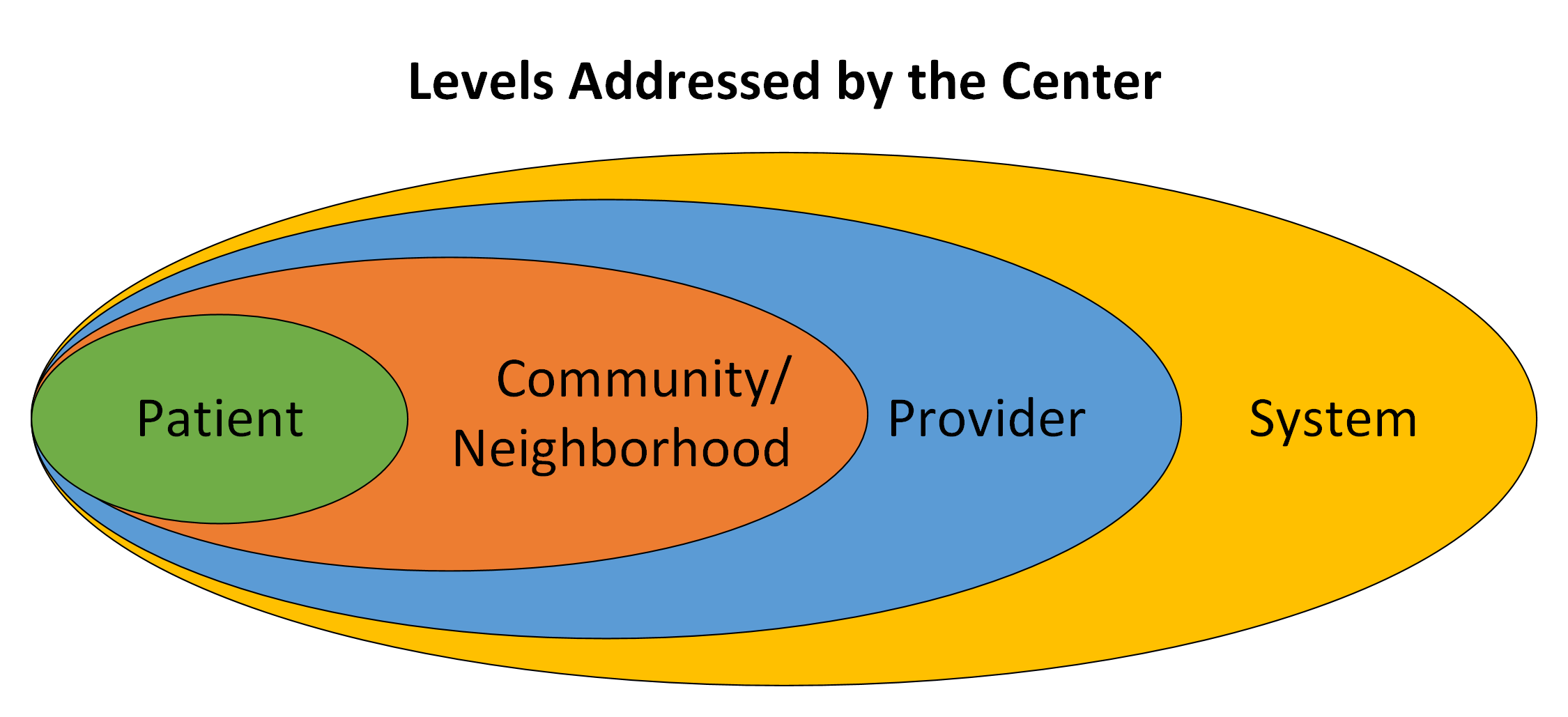
The Center’s groundbreaking work will be led by members of partnering communities and Michigan State University faculty. The work will reduce disparities by implementing and testing interventions to reduce maternal illness and death through three projects - each with novel designs covering the pregnancy through postpartum periods. These projects will all build off each other, address multiple levels needed to create meaningful change, and work across several health systems.
In addition to information on how well the projects are running, the Center will collect information on pregnancy-related death and a wide range of pregnancy-related illnesses. The Center will also have access to a linked Michigan Medicaid dataset. This connection will allow the Center to organize information across projects and other national Centers. The Center will use this information to find the main effects of each project, the combined effects across projects, and ways to sustain and scale-up the work.
This Center will address the need for multilevel, community-centered, equity-focused interventions developed and tested with an emphasis on scalability and sustainment to address disparities in pregnancy-related illness and death.
Primary Investigators
Cris Meghea, PhD
He/Him
Associate Professor of Obstetrics, Gynecology, and Reproductive Biology
Director and Co-Founder of the Advancing Maternal Health Equity LabJennifer E. Johnson, PhD
She/Her
C.S. Mott Endowed Professor of Public Health
Professor of OBGYN
Professor of Psychiatry and Behavioral MedicinePeggy Vander Meulen, MSN, RN
She/Her
Program Director of Strong BeginningsCenter investigators include Steve Ondersma, Claire Margerison, LeeAnne Roman, Kent Key, Alla Sikorskii, Jim Dearing, Rick Leach, Hannah Bolder, and Xiao Yu from MSU; Kimberlydawn Wisdom and Jaye Clement from HFH; Peggy Vander Meulen and Celeste Sanchez-Lloyd from Corewell Health; E. Hill De Loney and Sharon Saddler from Flint Community Based Organization Partners (CBOP), Athena McKay from Flint Innovation Solutions, and Bob Sokol from Wayne State University. The Center and every core have both academic and community PIs.
Community and health partners in MI and nationally include the Flint Community Based Organization Partners (CBOP), Hurley Medical Center, Munson Healthcare, MyMichigan Health, MDHHS, MiCHWA - Michigan
Community Health Worker Alliance, AIM CCI - Alliance for Innovation on Maternal Health—Community Care Initiative, and others.
This Center will reduce pregnancy-related and pregnancy-associated maternal morbidity and mortality (PRAMM) disparities in African American, Hispanic, and rural populations through innovative and culturally relevant community-partnered effectiveness and implementation research. The Center tests multilevel, community-centered, equity-focused interventions for PRAMM disparities, with an emphasis on scalability and sustainment. It is also home to a community partnership consortium and training program.
Project 1: Multilevel community-centered intervention to reduce pregnancy related and associated morbidity and mortality (PRAMM) disparities in non-Hispanic Black and Hispanic Medicaid-insured individuals.
Investigators: Meghea, Slaughter-Acey, and Wisdom
This project is the first large-scale test of a home visiting program that integrates community health workers to focus on PRAMM disparities issues, including comorbid conditions. It will address patient-provider interactions from provider and patient perspectives.
Project 2: High reach, multi-level digital intervention for pregnancy-related and -associated morbidity and mortality (PRAMM) disparities.
Investigators: Ondersma, Margerison, and McKay
This project develops and tests the effectiveness of a technology-enabled approached to reducing PRAMM disparities among rural and African American populations.
Project 3: Scale-up implementation approaches to ending pregnancy-related and -associated morbidity and mortality (PRAMM) disparities.
Investigators: Johnson and Clement
This project will develop and evaluate the effectiveness and cost-effectiveness of a scale-up implementation approach for scaling equity-focused outpatient and community care safety bundles county-wide in 12 Michigan counties with a population of nearly 6 million people.
Community Partnership Consortium
Investigators: Key and Sanchez-Lloyd
This Consortium will create an action-oriented, inclusive, broad-based stakeholder group to act as full partners in increasing the relevant and reach of Center activities.
Training program addressing the multilevel factors that affect pregnancy-related and pregnancy-associated morbidity and mortality disparities
Investigators: Margerison, Meghea, and Saddler
The Center will engage and prepare early-stage investigators, especially those from backgrounds or identities currently underrepresented in the health sciences, to conduct research that address the biological, behavioral, environmental, and structural determinants of PRAMM disparities.
The NIH press release:
https://www.nichd.nih.gov/newsroom/news/081723-Maternal-Health-Research-Centers
Release: NIH establishes Maternal Health Research Centers of Excellence
Initiative to support research to reduce pregnancy-related complications and deaths and promote maternal health equity
Credit: NICHDThe National Institutes of Health has awarded $24 million in first-year funding to establish Maternal Health Research Centers of Excellence. Part of NIH’s Implementing a Maternal health and PRegnancy Outcomes Vision for Everyone (IMPROVE) initiative, the centers will develop and evaluate innovative approaches to reduce pregnancy-related complications and deaths and promote maternal health equity. The grants are expected to last seven years and total an estimated $168 million, pending the availability of funds.
Compared to other high-income countries, the United States has a high rate of maternal deaths, with more than 1,200 such deaths occurring in 2021, the most recent year for which data are available. Each year tens of thousands more Americans experience severe pregnancy-related complications, which can raise the risk of future health concerns, including high blood pressure, diabetes and mental health conditions. There are stark disparities in these maternal health outcomes by racial and ethnic group, age, education, socioeconomic status and geographic region.
“The magnitude and persistence of maternal health disparities in the United States underscore the need for research to identify evidence-based solutions to promote health equity and improve outcomes nationwide,” says Diana W. Bianchi, M.D., director of NIH’s Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD). “Through collaborations with community partners and others, the Maternal Health Research Centers of Excellence will generate critical scientific evidence to help guide clinical care and reduce health disparities during and after pregnancy.”
NICHD, the NIH Office of Research on Women’s Health and the National Institute of Nursing Research co-lead the IMPROVE initiative, with involvement from several other components at NIH.
The centers of excellence include 10 research centers, a data innovation and coordinating hub and an implementation science hub. Together, these institutions will work to design and implement research projects to address the biological, behavioral, environmental, sociocultural and structural factors that affect pregnancy-related complications and deaths. They will focus on populations that experience health disparities, including racial and ethnic minorities, socioeconomically disadvantaged populations, those living in underserved rural areas, sexual and gender minority populations and people with disabilities.
Research centers will partner with community collaborators, such as state and local public health agencies, community health centers and faith-based organizations. Additionally, the research centers will support training and professional development of maternal health researchers, including those from backgrounds underrepresented in the biomedical research workforce.
Funding for the centers was awarded after a competitive peer review process. The following institutions, listed alphabetically along with project name and contact principal investigator, will participate as research centers:
- Avera McKennan Hospital, Sioux Falls, South Dakota
Maternal American-Indian Rural Community Health (MARCH)
Principal investigator: Amy J. Elliott, Ph.D.- Columbia University, New York City
NY Community-Hospital-Academic Maternal Health Equity Partnerships (NY-CHAMP)
Principal investigator: Uma Reddy, M.D.- Jackson State University, Jackson, Mississippi
Delta Mississippi Center of Excellence in Maternal Health
Principal investigator: Mary D. Shaw, Ph.D.- Medical College of Wisconsin, Milwaukee
Addressing Key Social-Structural Risk Factors for Racial Disparities in Maternal Morbidity in Southeastern Wisconsin (ASCEND WI)
Principal investigator: Anna Palatnik, M.D.- Michigan State University, East Lansing
Maternal Health Multilevel Intervention/s for Racial Equity (MIRACLE) Center
Principal investigator: Cristian Ioan Meghea, Ph.D.- Morehouse School of Medicine, Atlanta, Georgia
Center to Advance Reproductive Justice and Behavioral Health among Black Pregnant/Postpartum Women and Birthing People (CORAL)
Principal investigator: Natalie Dolores Hernandez, Ph.D.- Stanford University, Stanford, California
Stanford PRIHSM: Preventing Inequities in Hemorrhage-related Severe Maternal Morbidity
Principal investigator: Yasser Y. El-Sayed, M.D.- Tulane University, New Orleans
Southern Center for Maternal Health Equity
Principal investigator: Emily Wheeler Harville, Ph.D.- University of Oklahoma Health Sciences Center, Oklahoma City
Center for Indigenous Resilience, Culture, and Maternal Health Equity
Principal investigator: Karina M. Shreffler, Ph.D.- University of Utah, Salt Lake City
ELEVATE Center: Reduction of Maternal Morbidity from Substance Use Disorder in Utah
Principal investigator: Torri D. Metz, M.D.Johns Hopkins University, Baltimore, will serve as the data innovation and coordinating hub. Led by principal investigator Andreea Creanga, M.D., Ph.D., this hub will support data collection, ensure high data quality and provide data science expertise. The University of Pennsylvania, Philadelphia, will serve as the implementation science hub. Under the direction of principal investigator Meghan Brooks Lane-Fall, M.D., this hub will help to promote the integration of research findings and evidence into public health, clinical practice and community settings.
About the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD): NICHD leads research and training to understand human development, improve reproductive health, enhance the lives of children and adolescents, and optimize abilities for all. For more information, visit https://www.nichd.nih.gov .
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit https://www.nih.gov .
A Detroit Free Press story on the MIRACLE Center with some explosive quotes:
Michigan gets $19M federal grant to tackle racial health disparities in pregnant, new moms
By Kristen Jordan Shamus - October 12, 2023Researchers at Michigan State University, Henry Ford Health and Corewell Health are launching a new, $19 million research center aimed at reducing disparities in pregnancy-associated deaths among Black, Hispanic, American Indian/Alaska Native women, and those who live in rural areas of the Lower Peninsula.
Called the Multilevel Interventions to Advance Maternal Health Equity Center, or the MIRACLE Center, it's one of 10 nationally to win funding from the National Institutes of Health to address racial health disparities in maternal mortality. It also is the first of its kind in Michigan.
"It is absolutely appalling to see the rates (of maternal mortality) that this country has experienced, given the wealth and the resources that we have," said Peggy Vander Meulen, director of Kent County’s Strong Beginnings, manager of community health programs at Corewell Health and a co-leader of the MIRACLE Center.
Researchers at Michigan State University, Henry Ford Health and Corewell Health are collaborating to launch a new, $19 million research center aimed at reducing disparities in pregnancy-associated deaths among Black, Hispanic, American Indian/Alaska Native women, and those who live in rural areas of the Lower Peninsula.
"What is the most upsetting is not only that maternal mortality overall has increased, but the rising disparities and inequities, particularly for Black and indigenous persons and also for Latino persons."
The underlying driver, she said, is "the systemic, institutionalized and structural racism that is been intentionally woven into the fabric of the society from the very beginning, and continues to intentionally or unintentionally result in inequities."
It affects everything from employment opportunities to access to safe and affordable housing, transportation and child care — and increases the risk that a woman will die during pregnancy and in the year after a baby is born, Vander Meulen said.
Black women 2.8 times more likely to die of pregnancy-related causes
In Michigan, the state Department of Health and Human Services reports that of the 80-90 maternal deaths that occur each year, 64% are preventable.
Black women in Michigan were 2.8 times more likely to die from pregnancy-related causes in 2015-19 than white women. The maternal mortality rate for Black women was 29.8 per 100,000 live births. For white women, it was 10.7 deaths per 100,000 live births, according to state data.
"The cause of all the disparities are racism, racism and racism," said Jennifer Johnson, C.S. Mott Endowed professor of public health in the MSU College of Human Medicine, and a co-leader of the MIRACLE Center.
"We're looking at two different kinds of disparities: One is the direct medical causes. Another is suicide, overdose, homicide. I think people are clear (in understanding) how the suicide, overdose, homicide deaths are responses to life stress. But more than half of the deaths occur after birth. ... If a mom is just trying to make ends meet, she may not go back for a two-week or a six-week checkup or she may be having headaches or she may be having shortness of breath. These other concerning symptoms and just sort of shake off or think, 'Oh, I don't have time for this' and then she dies."
Support for new mothers falls short
Exacerbating the problem is a lack of support for families, Vander Meulen said.
"People talk a great line about family values. However, we don't have ... mandatory parental leave or affordable child care," she said. "How do we expect parents and children to thrive? We have clients going back to work two weeks after delivery because they can't afford the time off. They can't afford to miss work at the minimum-wage jobs they're working just to keep food on the table."
Peggy Vander Meulen, director of Kent County’s Strong Beginnings and manager of community health programs at Corewell Health, is among the leaders of a new, $19 million project to study and reduce racial health disparities among pregnant and post-partum women in Michigan.
The rate of maternal mortality in Michigan more than doubled from 2018 to 2019 to a rate of 23.2 pregnancy-related maternal deaths per 100,000 live births. Official data on maternal mortality in Michigan for 2020, the first year of the coronavirus pandemic, won’t be released until early 2024, state health officials told the Free Press for a previous story.Access to health care also is a problem, both in rural parts of the state as well as urban centers, said Cristian Meghea, an associate professor of obstetrics, gynecology and reproductive biology in the MSU College of Human Medicine and co-leader of the MIRACLE Center.
"Having Medicaid insurance, that's great," Meghea said. "However, securing access to care and having an OB-GYN or even a general practitioner accepting new patients on Medicaid, that's a whole different problem. And a third problem is reaching that provider ... without having a car or without having reliable bus transportation. Or, being late and then getting your appointment canceled. These are all multiple hoops that that a lot of women have to go through."
Cristian Meghea, an associate professor of obstetrics, gynecology and reproductive biology in the Michigan State University College of Human Medicine and co-leader of the MIRACLE Center.
More:At least 60% of maternal deaths in Michigan are preventableAccess to care isn't enough. Women also need respect
Johnson added that even when people overcome all those barriers, they may face overt or implicit racism in the doctor's office.
"Once you get there, there's a respect issue. Am I being listened to? Am I being heard? Am I being respected when I voiced my concerns? Is my partner being respected when he joins me or when he is unable to join me?
Jennifer Johnson is a C.S. Mott Endowed professor of public health in the Michigan State University College of Human Medicine, and a co-leader of the MIRACLE Center.
"And so you have all these layers that contribute to mom saying, 'Well, yeah, I can find a provider. I have one, but when I go, I'm being so disrespected, I don't want to go. I'm willing to just wait it out until delivery and just show up to the emergency room.' And so that's another component of how do we make sure we're getting women not just access to care, but the proper and respected care that they deserve?"The center is launching three projects that begin immediately and will continue for seven years across 20 counties in the Lower Peninsula.
Project 1: Community health workers, visiting nurses and social workers will periodically visit the homes of pregnant and postpartum Black and Hispanic women in Kent, Wayne and Genesee counties to coordinate community and clinical care.
Project 2: Expands the use of a self-screening digital application that pregnant Black women and women living in rural areas can use to identify health warning signs. They can use it to live chat with community health workers who can connect them with services in 10 counties: Kent, Genesee, Ingham, Isabella, Emmet, Grand Traverse, Otsego, Alpena, Midland and Gratiot.
Project 3: Works to identify the best ways to improve equity in maternal care across 14 Michigan counties, focusing on improvement in the quality of care in both the medical setting and within the community. The counties involved are: Genesee, Kent, Wayne, Oakland, Ingham, Isabella, Macomb, Muskegon, Calhoun, Jackson, Saginaw, Kalamazoo, Berrien and Washtenaw.
"It is possible to improve the overall quality of obstetric care without changing disparities," Johnson said. "What Project 3 does is it looks at quality improvement efforts, targeting outpatient care and community care, and enhanced prenatal care because that's where most of the deaths occur. It looks at quality improvement approaches that directly target disparities.
"Despite some of the biases, white moms are actually more likely to die by overdose in pregnancy and postpartum than African American moms. But our African American moms are much more likely to die by homicide. As a matter of fact, for African-American women, the risk of dying by partner violence while pregnant increases eight fold.
"In general, if a woman dies, more than half the time it is by a current or former partner. Most of the deaths ... are suicide, overdose, homicide.
The MIRACLE Center will work through partnerships among university researchers, doctors, nurses and others at Henry Ford Health, Corewell Health, the Flint Community Based Organization Partners, Flint Odyssey House, Hurley Medical Center, Munson Healthcare, MyMichigan Health, and the Michigan Department of Health and Human Services.