This bad news is likely to provoke a slew of new health care policies at all levels of government and industry:
https://www.cdc.gov/nchs/data/vsrr/vsrr033.pdf
Infant Mortality in the United States: Provisional Data From the 2022 Period Linked Birth/Infant Death FileBy Danielle M. Ely, Ph.D., and Anne K. Driscoll, Ph.D
Abstract
Objectives—This report presents provisional 2022 data on infant mortality rates using the U.S. linked birth/infant death files. Infant mortality rates are shown by infant age at death, maternal race and Hispanic origin and age, gestational age and sex of the newborn, state of residence of the mother, and 10 leading causes of infant death.
Methods—Data are from the period linked birth/infant death files, which link infant deaths with the corresponding birth certificates. Comparisons are made between provisional 2022 and final 2021 data. The linked birth/infant files are based on 100% of birth certificates and 98%–99% of infant death certificates registered in all states and the District of Columbia. For 2022, 1.4% of infant deaths remained unlinked. Infant deaths in states with less than 100% of infant death records linked to their respective birth records are weighted.
Results—The provisional infant mortality rate for the United States in 2022 was 5.60 infant deaths per 1,000 live births, 3% higher than the rate in 2021 (5.44). The neonatal mortality rate increased 3% from 3.49 to 3.58, and the postneonatal mortality rate by 4% (from 1.95 to 2.02) from 2021 to 2022. Mortality rates increased significantly among infants of American Indian and Alaska Native non-Hispanic (7.46 to 9.06) and White non-Hispanic (4.36 to 4.52) women. From 2021 to 2022, infant mortality rates increased significantly for infants of women ages 25–29, from 5.15 to 5.37. Mortality rates increased significantly for total preterm (less than 37 weeks of gestation) and early preterm (less than 34 weeks of gestation) infants. The mortality rate increased significantly only for male infants from 2021 to 2022. Infant mortality rates increased in four states and declined in one state. Mortality rates increased for 2 of the 10 leading causes of death: maternal complications and bacterial sepsis.
<snip>
Summary
The infant mortality rate for the United States rose 3% from 2021 to 2022, the first year-to-year increase in the rate since 2001 to 2002 (6). From 2002 to 2021, the infant mortality rate declined 22%. From 2021 to 2022, increases in mortality rates were observed for neonatal and postneonatal infant deaths, infants born to American Indian and Alaska Native and White women, and infants born to women ages 25–29. Rates also increased for infants born preterm, male infants, and for infants in four states (Georgia, Iowa, Missouri, and Texas). Mortality rates increased significantly for 2 of the 10 leading causes of death: maternal complications and bacterial sepsis.
Although not statistically significant, rates generally increased for most other race and Hispanic origin, maternal age,
and gestational age groups, as well as for female infants, in a majority of states, and for 3 of the 10 leading causes of
death.
Just imagine how high that number would be if they factored in abortions!
And it doesn't stop there.
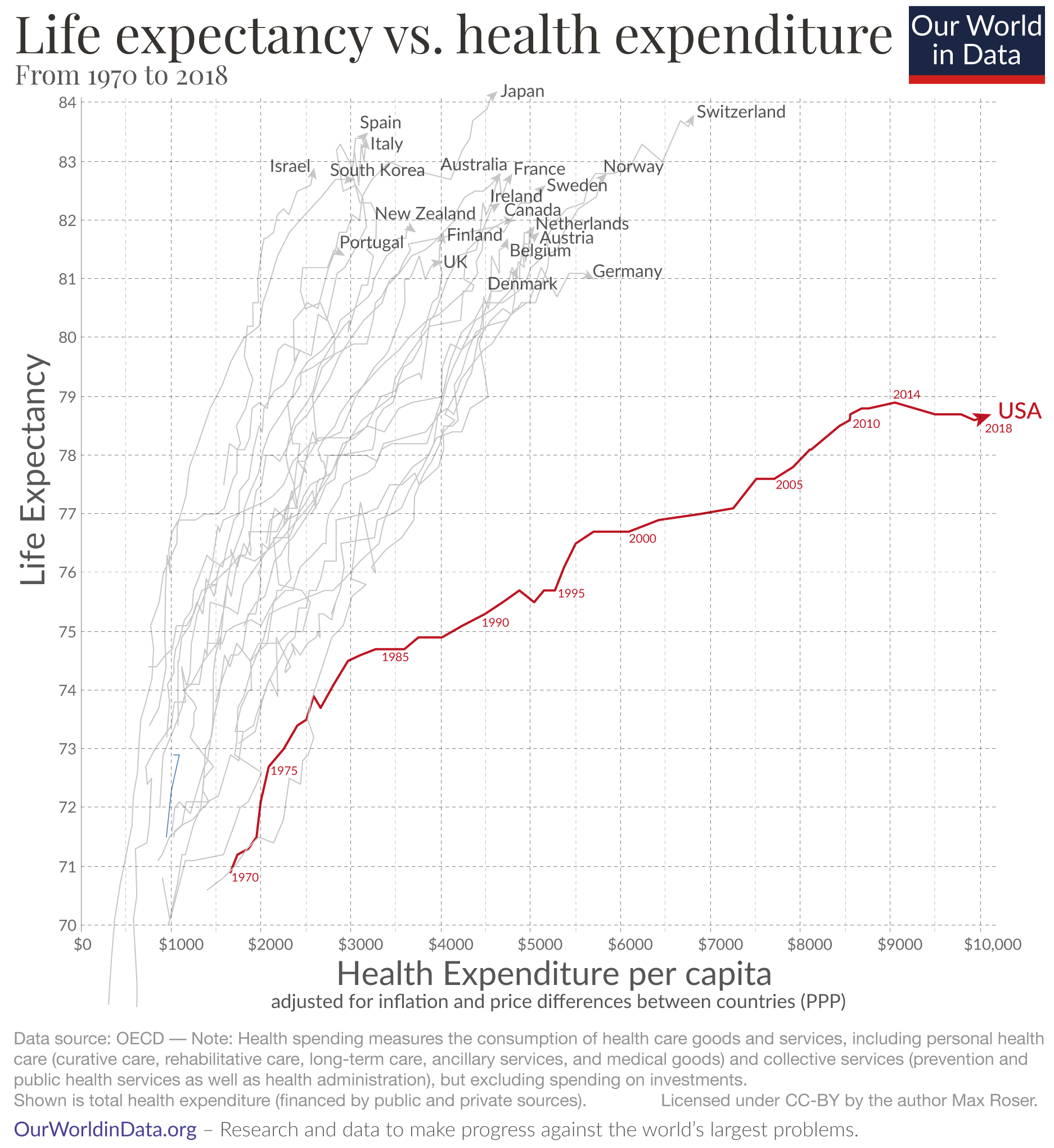
Sure, there are all sorts of contributing factors, but notice the date of the US inflection point in this 2020 comparison of life expectancy and health expenditure.
Significantly, 2014 was the year we switched clinical attention from individuals, to systems.
The Obamacare leap in federal spending, control, and redirection from patients to data is losing US lives before their time.
Why is life expectancy in the US lower than in other rich countries?
Americans have a lower life expectancy than people in other rich countries despite paying much more for healthcare. What factors may explain this?
Why do Americans have a lower life expectancy than people in other rich countries, despite paying so much more for health care?
The short summary of what I will discuss below is that Americans suffer higher death rates from smoking, obesity, homicides, opioid overdoses, suicides, road accidents, and infant deaths. In addition to this, deeper poverty and less access to healthcare mean Americans at lower incomes die at a younger age than poor people in other rich countries.
Life expectancy and health expenditure over time, the US is an outlier
The US clearly stands out as the chart shows: Americans spend far more on health than any other country in the world, yet the life expectancy of the American population is shorter than in other rich countries that spend far less.
The chart here doesn’t just show the latest data points, but how life expectancy and health spending have changed during the last five decades. The arrows start in 1970 and connect the annual data points for both metrics, showing the change over time.
In the 1970s the US didn’t stand out at all, it does so now because life expectancy increased much more slowly than in other countries. At the same time, health spending in the U.S. increased much more rapidly, particularly since the mid-1980s. The consequence of these two exceptional developments is that the US followed the much-flatter trajectory that the chart shows.
The unequal development over recent decades led to an inequality between the US and other rich countries. In the US health spending per capita is up to four times higher, yet life expectancy is lower than in all of these countries.
The US has achieved very substantial progress in health outcomes over the last 140 years: in 1880 the life expectancy of Americans was 39 years, since then it has doubled. But this extremely positive trend has come to an end. While life expectancy for people around the world continued to increase, the life expectancy of Americans has declined since 2014. With the pandemic of 2020 – which already caused more than 225,000 deaths due to COVID-19 and 300,000 excess deaths – it is unfortunately already certain that the decline of life expectancy in the US will continue this year.1
It appears that the central claim of this CDC report is another DEI infused fraud. Gail L. Heriot, a member of the U.S. Commission on Civil Rights, posted a paper on SSRN in 2021, observing that that changes in death certificates have caused more deaths to be classified as maternal in nature. Hence the increase in reported maternal death rates:
https://papers.ssrn.com/sol3/Delivery.cfm/SSRN_ID3942067_code514132.pdf?abstractid=3924645&mirid=1
AbstractOn September 15, 2021, the U.S. Commission on Civil Rights published a report entitled Racial Disparities in Maternal Health (the “Report”). This Dissenting Statement and Rebuttal (the “Statement”) is a part of that report.
Among other things, the Statement points out several errors in Report. For example, the Report incorrectly states that maternal mortality has increased 50% over the last generation. What has actually happened is that changes in death certificates have caused more deaths to be classified as maternal in nature. The Report also emphasizes the theory that racism plays a prominent role in causing racial disparities in maternal mortality. The Statement points out in response that maternal mortality rates for Hispanic and Asian American mothers are lower than the rate for white mothers. This tends to detract from the theory that racism is what’s causing the disparities.....