- To Lead Health Care Well, Physicians Must Learn the System
- Bassett Healthcare Network appoints division chief of dental services
- Why this CIO treated an EHR decision as an operating model reset
- For-profit operators: 43 executive moves in 2026
- HCA Florida hospital names CFO
- Aetna fined $550K for mental health parity violations
- 10 states with lowest, highest dental costs
- Sutter launches neonatal transport program with $10M gift
- BayCare hospital taps new operations leader
- Surgery Partners revenue hits $3.3B in 2025
- Altru completes CommonSpirit hospital acquisition
- Henry Ford hospital nurses strike hits 6-month mark: 4 notes
- Cigna COO to succeed retiring predecessor as CEO
- Staffing mandates won’t cause SNF closures: Study
- Why CommonSpirit is exiting Conifer
- How the hygienist shortage will shape the future of dentistry
- Humana expands cardiac care partnerships for Medicare Advantage
- Virginia physician group acquired after 25+ years of independence
- Principal acquires largest dental network in Alabama
- Why private practice will survive in the DSO era
- ‘We’re running in when others are running out’: Stability drives record growth for regional Medicare Advantage plans
- California provider opens teen mental health center
- Idaho GI group cuts appointment wait times with virtual platform
- 6 Texas physicians to pay $5M to settle false claims allegations
- Inside Huntsman’s hybrid model boosting social worker capacity sixfold
- 12 dental technology updates to know
- Imagen Dental Partners adds California practice
- South Carolina’s largest independent multispecialty group acquired
- Gastroenterology and private equity in 2026: 5 notes
- WHO calls for environmentally friendly, less invasive dental care: 5 notes
- The GI physician shortage by state, by 2036
- ASC vs. HOPD costs for 5 orthopedic procedures
- HCA Healthcare says all-time high inpatient capacity, ACA exchange attrition won't spoil 2026 volume growth
- Federal lawmakers introduce bill to reverse Medicaid cuts, expand Medicare dental coverage: 4 notes
- Maryland awards $1.6M for substance use disorder, peer recovery workforce expansion
- Pfizer CEO Albert Bourla on FDA official Vinay Prasad: 'We have a problem with the leadership of CBER'
- SSM Health adds gastroenterologist
- San Diego provider opens 32-bed residential mental health facility
- AI Therapist? It Falls Short, a New Study Warns
- Nevada hospital to downsize, switch to rural emergency status
- Mental health providers subject to ban on youth ‘transition’ procedures: Texas attorney general
- Moody’s downgrades Arkansas system’s credit rating
- Innovate 32 continues growth, adds 2 dental practices in Tennessee
- Grow Therapy scores $150M to build out enterprise partnerships with docs, employers
- Indiana hospital transitions revenue cycle operations to Revology
- Mayo Clinic posts 6.8% margin in 2025
- Nearly 20 States Scale Back HIV Medication Programs
- BBQ Sauce Recall Issued Nationwide Due To Incorrect Label
- FDA Recalls More Than 651,000 Jugs of Water Over Sanitation Concerns
- Listen to the Latest ‘KFF Health News Minute’
- Corewell Health posts 1.6% operating margin, grows revenue to $17.6B — 7 things to know
- Hasta los pacientes se sorprenden por los precios que sus aseguradoras están dispuestas a pagar, un costo que al final pagamos todos
- Patients with multiple chronic diseases are a looming threat to health systems' financials: Vizient
- Guardant picks Patrick Dempsey for colorectal cancer blood test awareness
- Breast Cancer Cases, Deaths Expected To Rise Worldwide
- Collagen Supplements Good For Skin, Arthritis, Evidence Review Concludes
- Illicit Adderall Use Places Stress On The Heart, Study Shows
- A-Fib Drug, Diltiazem, Could Interact With Blood Thinners, Increase Risk Of Dangerous Bleeding
- How to Get Ready For Daylight Saving Time
- Effective Sunscreen Protection Can Cost $40 A Year
- Longtime Cigna CEO David Cordani to retire, Brian Evanko tapped as successor
- Acadia, undaunted by recent EU rejection, seeks CHMP re-examination of Rett syndrome med Daybue
- FDA’s CRLs reveal critical errors in AstraZeneca’s Saphnelo data, efficacy doubts for GSK’s Exdensur
- Even Patients Are Shocked by the Prices Their Insurers Will Pay — And It Costs All of Us
- Readers Lean On Congress To Solve Crises in Research and Rehab
- Federal Aid for Lead Cleanup Is Receding. That’s a Problem for Cash-Strapped Cities.
- Disc lays off 20% of employees to steady ship after FDA rejection of rare disease drug
- Novo plugs $500M into Ireland plant to produce Wegovy pill for markets outside US
- Esperion pays $75M-plus to acquire Corstasis and newly approved Enbumyst
- Children’s Mercy raises $150M for mental healthcare
- California awards $291M to expand behavioral health housing, services
- OhioHealth builds well-being programs to reshape caregiver culture
- Lawmakers introduce bill to reverse Medicaid cuts, expand Medicare benefits
- 100+ organizations call on CMS to revise 2027 MA rates
- UNC Health Appalachian offers psychiatric physician training program
- UHS to roll out behavioral health revenue cycle AI tools in 2026
- In 1 state, large hospitals dominate 340B's net savings
- HHS bans Claude AI tool as Trump seeks full government blacklisting of Anthropic
- Report: Most states investing in value-based care with Rural Health Transformation Program
- U.S. Tops 1,100 Measles Cases This Year as Outbreaks Grow
- FDA To Offer Cash Bonuses for Faster Drug Reviews
- 'One2PrEP': Gilead's 1st Yeztugo DTC ad reimagines hit song to highlight biannual dosing
- GLP-1s support heart attack recovery in rodents by relaxing tight blood vessels
- Former Optum CEO Heather Cianfrocco to depart UnitedHealth Group
- New Drug, Acoziborole, Could Boost Efforts to Wipe Out Sleeping Sickness
- Chocolate Male Supplement Recalled Over Hidden Erectile Dysfunction Drug
- Amid unfolding Middle East war, pharma giants keep close eye on employee safety, supply chains
- CMS set to suspend enrollment in Elevance Health's Medicare Advantage plans
- Providers urge Education Department to reconsider which jobs face stiffer student loan caps
- Kennedy adds 2 new members to CDC’s vaccine panel ahead of delayed meeting
- Kennedy adds 2 new members to CDC’s vaccine panel ahead of delayed meeting
- Urban Traffic Noise Disrupts Sleep, Affects Heart Health After One Night
- Hormone Therapy Might Be Unnecessary For Some Prostate Cancer Patients
- Benzodiazepine Use Down In U.S., But OD Risk Remains, Study Says
- GLP-1 Drugs Might Ease Chronic Migraine, Study Says
- Blood Test Reveals Alcohol-Related Liver Disease
- Telemedicine Visits Cost Five Times Less Than In-Clinic Care
- Medicaid Is Paying for More Dental Care. GOP Cuts Threaten To Reverse the Trend.
- Families Defend Disability Services Amid Medicaid Cuts
- Bavarian Nordic CEO to follow board chair out the door after failed private equity takeover
- Ascendis gains more altitude with FDA approval for dwarfism drug Yuviwel
- CDMO Quotient extends Ipsen supply pact for rare disease drug Sohonos
- Quest Diagnostics launches Google-powered AI chatbot to help patients understand lab results
- Tennr takes aim at phone call bottlenecks as it builds out automation for patient referral process
- DoseSpot, Arrive Health merge to combine prescribing tools with pharmacy, medical benefit data
- Why Digital Tool are Needed to Cope with Increasing Pressures in MedTech Innovation
- Why Digital Tool are Needed to Cope with Increasing Pressures in MedTech Innovation
- Electronics Pollution Pose Added Threat to Endangered Dolphins, Porpoises
- Flea And Tick Pills May Pose Environmental Risks, Study Finds
- ICE, ALS, Addiction Medicine, and Robotic Ultrasounds: Journalists Sound Off on All That and More
- A Canadian Hospital Scoops Up Nurses Who No Longer Feel Safe in Trump’s America
- Statement on the Adoption of Final Rules Under the Holding Foreign Insiders Accountable Act
- Statement on Final Rules for the Holding Foreign Insiders Accountable Act
- State Medicaid budgets to weather $664B reduction through 2034 due to OBBBA: RAND
- Clover Health CEO said company sees opportunity in complex MA environment
- How pharma marketers are capturing the power of podcasts to connect with consumers
- Cigna's Evernorth quietly acquires hospital pharmacy CarepathRx
- Walgreens debuts virtual weight management clinic with access to GLP-1 meds
- New Obamacare Rules Could Raise Deductibles to $31K For Families
- Study Suggests One Common Amino Acid May Affect How Long Men Live
- Merck to wind down Gardasil production at N.C. plant, lay off 150-plus
- Walmart Great Value Cottage Cheese Recalled Over Pasteurization Issue
- Chris Bosh Says He’s 'Lucky To Be Alive' After Sudden Health Scare
- Patrick Kennedy: Collab with MAHA is essential to address mental health crisis
- Lilly debuts Nvidia supercomputer with fanfare and focus on escaping traditional pharma lifecycle
- Alignment CEO John Kao offers measured response to proposed 2027 MA rates
- Sanofi, Genentech, Kedrion back star-studded bleeding disorder awareness campaign
- Op-ed: Our patients deserve better safety reporting. AI could be the answer
- How the Brain Learns to Have Seizures During Sleep
- Blood Test Can Predict Short-Term Survival Among Seniors
- Why Turning 19 Spikes Medicaid Loss for Millions
- Crash Course Might Speed Brain Stimulation Treatment For Depression, Study Suggests
- Wildfire Smoke Linked To Increase In Violent Assaults
- More Parents Are Refusing A Life-Saving Shot For Their Newborns, Study Finds
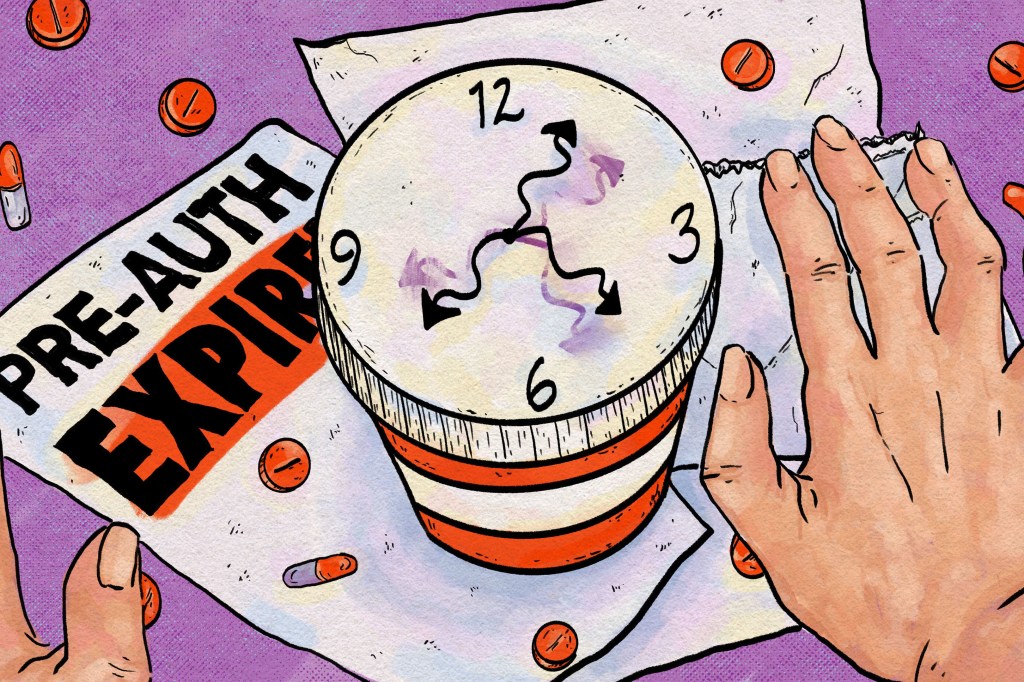
- To Avoid Care Disruptions, Know When the Clock Runs Out on Your Prior Authorization
- Lake Nona Impact Forum: There can't be longevity without tech
- FDA Approval for BIOTRONIK Solia CSP S Pacing Lead For LBBAP
- FDA Approval for BIOTRONIK Solia CSP S Pacing Lead For LBBAP
- Catalyst OrthoScience gets FDA 510(k) Clearance of Archer® Patient-Specific Instrumentation for Shoulder Arthroplasty
- Catalyst OrthoScience gets FDA 510(k) Clearance of Archer® Patient-Specific Instrumentation for Shoulder Arthroplasty
- Smith+Nephew signs distribution agreement with SI-BONE
- Smith+Nephew signs distribution agreement with SI-BONE
- Quantum Surgical Acquires NeuWave Medical, Inc.
- Quantum Surgical Acquires NeuWave Medical, Inc.
- Partnering to Advance Drug Delivery Innovation
- How Pharma is Expanding its Global Footprint to Advance Clinical Research
- Stryker launches Synchfix™ EVT, expanding options for flexible syndesmotic fixation
- Stryker launches Synchfix™ EVT, expanding options for flexible syndesmotic fixation
- Democrat-Led States Sue Trump Administration Over Cuts to Childhood Vaccine Schedule
- CDC Vaccine Advisory Panel To Revisit COVID Shot Safety Next Month

Priority Health is Michigan's second-largest health insurer. In this longform report, ProPublica breaks the story of its particularly shameful episode of healthcare greed.
A must-read for Michigan residents. Excerpted here for length.
https://www.propublica.org/article/priority-health-michigan-cart-insurance-vanpatten-denials
Insurance Executives Refused to Pay for the Cancer Treatment That Could Have Saved Him. This Is How They Did It.
A Michigan law requires coverage of cancer drugs. One insurer came up with a “defensible” way to avoid paying for treatments that offered Forrest VanPatten his last chance for survival. “We crossed the line,” says a former executive.
Forrest VanPatten was 50 and strong after years as a molten-iron pourer when he learned in July 2019 that a hyperaggressive form of lymphoma had invaded his body. Chemotherapy failed. Because he was not in remission, a stem cell transplant wasn’t an option. But his oncologist offered a lifeline: Don’t worry, there’s still CAR-T.
The cutting-edge therapy could weaponize VanPatten’s own cells to beat back his disease. It had extended the lives of hundreds of patients who otherwise had no chance. And VanPatten was a good candidate for treatment, with a fierce drive to stay alive for his wife of 25 years and their grown kids.
He and his family gripped tight to the hope that the treatment promised.
Then, his insurance company refused to approve it.
Across the country, health insurers are flouting state laws like the one in Michigan, created to guarantee access to critical medical care, ProPublica found. Fed up with insurers saying no too often, state legislators thought they’d solved the problem by passing hundreds of laws spelling out exactly what had to be covered. But companies have continued to dodge bills for pricey treatments, even as industry profits have risen. ProPublica identified dozens of cases in which plans refused to pay for high-stakes treatments or procedures — from emergency surgeries to mammograms — even though laws require insurers to cover them.
Like most policyholders, VanPatten had no insight into the decision made by his insurer, a nonprofit called Priority Health that covers about a million Michigan residents.
He didn’t know that around the time the therapy won the Food and Drug Administration’s approval, executives at Priority Health had figured out a way to weasel out of paying for it.
...
Co-published with The Capitol Forum
Series:Uncovered: How the Insurance Industry Denies Coverage to Patients
Health insurers reject millions of claims for treatment every year in America. Corporate insiders, recordings and internal emails expose the system and its harm.
ProPublica is a nonprofit newsroom that investigates abuses of power. Sign up to receive our biggest stories as soon as they’re published.
This story is part of a partnership with Scripps News.
A little-known fact about health insurance is its departure from enforceable contracts. As this story and countless denials prove, specific coverage mandates (like Michigan's for cancer drugs) are a poor substitute.
The ACA did away with stable contracts when it federalized coverage mandates. Since then, coverage details shift constantly and, for all intents and purposes, are unknowable by patients and doctors.
Ironically, the only aspect of healthcare that the US Constitution actually addresses is to prohibit state impairment of contracts.
State Senator Jeff Irwin (D-Ann Arbor) will file a bill to to reinforce Michigan’s existing cancer treatment mandate which requires State regulated health insurance plans to cover all new genetic therapies. DIFS hasn't cited a single Michigan insurer for violating this mandate since its inception in 1989:
https://www.propublica.org/article/michigan-state-health-plans-cancer-treatments
Michigan Lawmaker to Introduce Bill Requiring State Health Plans to Cover Cutting-Edge Cancer TreatmentsAfter ProPublica reported on a Michigan insurer that wouldn’t cover a cancer patient’s last-chance treatment, a state lawmaker said he would introduce a measure compelling health plans to cover a new generation of advanced cancer therapies.
By Robin Fields and Maya Miller - March 5, 2024
Spurred by a ProPublica story about an insurer that denied coverage of the only therapy that could have saved the life of a 50-year-old father of two, a Michigan lawmaker plans to introduce a bill Tuesday requiring health plans in the state to cover cutting-edge cancer treatments.
In February 2020, Forrest VanPatten died fighting Priority Health, one of Michigan’s largest health insurers, over its refusal to pay for CAR-T cell therapy, his last-chance treatment. The therapy works by genetically reengineering patients’ own cells, then infusing them back into the body to beat back their disease.
Michigan has long required insurers to cover proven cancer treatments, but according to internal emails, some Priority Health executives argued that CAR-T was a gene therapy, not a drug, and thus not subject to the state’s coverage mandate.
State Sen. Jeff Irwin, D-Ann Arbor, plans to file the new bill to make explicit that Michigan’s cancer treatment coverage mandate includes a new generation of genetic and immunotherapies, including CAR-T.
Earlier this year, Michigan’s top insurance regulator told health plans they had to cover these treatments. Irwin’s measure would codify that guidance, ensuring it’s not dependent on one regulator’s interpretation of the law. He said he wanted the state’s requirements to be abundantly clear to both patients and insurers.
“I feel that the insurance company in this case was painting outside the lines,” Irwin said Monday in an interview. “This change that we’re making, I think, is going to make it hard to impossible for someone to make that same decision again around these particular treatments.”
The bill’s introduction was bittersweet for the VanPatten family. “If this helps any other family, any other person, we are all for it,” said Betty VanPatten, Forrest’s widow. “It just feels like they got one over on everybody.” Betty and her children said they hope Priority Health faces repercussions for the decision to deny coverage for Forrest’s treatment.
Priority Health’s decision not to pay for CAR-T cancer treatments was almost entirely motivated by the medication’s high cost, former employees told ProPublica. “It was, ‘This was really expensive, how do we stop payment?’” recalled Dr. John Fox, Priority Health’s associate chief medical officer at the time.
When the Food and Drug Administration approved the first CAR-T therapy in 2017, Fox tried unsuccessfully to persuade executives at Priority Health to cover it, citing Michigan’s law. He left his position with the health plan in 2019, in large part because he was disillusioned with the company’s decision not to pay for life-prolonging cancer therapies.
In an earlier statement to ProPublica, Priority Health said that “there was a lack of consensus in the medical community regarding the treatment” when it was first approved, and that the company began offering coverage after “extensive clinical work improved the treatment.” But well before VanPatten’s doctors requested Priority Health’s approval for the treatment in early 2020, an alliance of leading U.S. cancer treatment centers concluded there was substantial consensus about the treatment’s efficacy.
Asked about Irwin’s bill, Priority Health spokesperson Mark Geary said in a written statement that the company complies with all existing federal and state laws and has been providing coverage for CAR-T cell therapy for several years. “We also stand ready to continue to work with lawmakers and regulators in Michigan to find ways to offer Michiganders affordable access to effective, evidence-based treatments and procedures,” Geary wrote.
In the aftermath of ProPublica’s story, several Michigan lawmakers called out the state’s insurance department for not investigating Priority Health’s actions in the VanPatten case and failing to enforce the law that requires coverage of cancer drugs.
Regulators acknowledged they hadn’t cited a single Michigan insurer for violating the mandate since it was created in 1989.
Under existing law, the Michigan Department of Insurance and Financial Services can levy fines against insurers that fail to comply and can even suspend or revoke their licenses.
In an emailed statement, Communications Director Laura Hall said the agency anticipated backing Irwin’s proposal. The department, she wrote, “supports efforts to embed protections for cancer patients in state law.”
If Irwin’s proposal passes, not all Michigan health plans will have to follow it. Some employers pay directly for workers’ health care, hiring insurers to process claims. These plans are regulated by the federal government and are exempt from state coverage requirements, though some follow them voluntarily.
The FDA is now having second thoughts about the efficacy of CAR-T therapies, especially in newly discovered cases of blood cancers. There are also significant safety concerns. This despite six different CAR-T therapies having been approved by FDA in 2017:
US FDA staff raise concerns over data from J&J, Bristol's CAR-T therapies
By Bhanvi Satija and Sneha S K - March 13, 2024March 13 (Reuters) - The U.S. Food and Drug Administration's staff on Wednesday raised concerns that it was unclear if Johnson & Johnson (JNJ.N) and Bristol Myers Squibb's (BMY.N) cell therapies would benefit blood cancer patients when given as early treatments.
Regulatory approval for the therapies as earlier treatments could expand their use to a larger subset of blood cancer patients who are less sick than those treated with multiple therapies. The therapies - J&J's Carvykti and Bristol's Abecma - belong to class known as CAR-T.
"I think there is a need for these therapies as patients are relapsing earlier," said Eric Smith from Boston's Dana Farber Cancer Institute.
FDA's staffers pointed to a pattern of early deaths in late-stage trials of the therapies, saying that it raised questions over the effectiveness of the treatments in extending the time patients live after receiving them.
Carvykti and Abecma are approved by the FDA to treat patients with multiple myeloma who have received at least four prior lines of treatment.J&J partners with Legend Biotech (LEGN.O), while 2seventy bio (TSVT.O) is Bristol's partner for Abecma.
Guggenheim analyst Kelsey Goodwin said the FDA's stance was harsher-than-expected, but expects both therapies to gain approval.
In late-stage studies, both the treatments helped extend the time patients live before their disease begins to worsen.
About 8% of trial patients died after receiving Carvykti or Abecma - a proportion higher than those being treated with standard of care therapies.
While data for Carvykti does not clearly establish the need for an additional trial, further overall survival data from Abecma may not be sufficient to overcome the risk of early deaths, the reviewers said.
J&J said it remained confident in the clinical profile of Carvykti.
The meeting of FDA's independent advisers set for Friday will be closely watched by investors to understand the regulator's view on CAR-T therapies, after recent safety concerns over the treatments.
Does anyone see a bright line between FDA and industry any more?
All I see is Pharma hauling on one end of the rope, Insurance on the other, and FDA suspended in the middle pretending to serve the public interest.
Get MHF Insights
News and tips for your healthcare freedom.
We never spam you. One-step unsubscribe.