- Mayo Clinic posts 6.8% margin in 2025
- Listen to the Latest ‘KFF Health News Minute’
- FDA clears AI tool to predict delivery date
- Corewell Health posts 1.6% operating margin, grows revenue to $17.6B — 7 things to know
- Corewell Health posts 1.6% operating margin, grows revenue to $17.6B — 7 things to know
- Woodside Health acquires Arizona facility
- New York safety-net hospital board chair to resign after 10 months
- New York physician sentenced to 7 years for unlawful drug distribution
- Hasta los pacientes se sorprenden por los precios que sus aseguradoras están dispuestas a pagar, un costo que al final pagamos todos
- Cooper University Health Care Selects hellocare.ai as Enterprise Platform for AI-Assisted Intelligent Hospital Rooms, Virtual Nursing, and Virtual Sitting
- How to Get Ready For Daylight Saving Time
- A-Fib Drug Could Interact With Blood Thinners, Increase Risk Of Dangerous Bleeding
- Collagen Supplements Good For Skin, Arthritis, Evidence Review Concludes
- Effective Sunscreen Protection Can Cost $40 A Year
- Illicit Adderall Use Places Stress On The Heart, Study Shows
- Breast Cancer Cases, Deaths Expected To Rise Worldwide
- Even Patients Are Shocked by the Prices Their Insurers Will Pay — And It Costs All of Us
- Readers Lean On Congress To Solve Crises in Research and Rehab
- Federal Aid for Lead Cleanup Is Receding. That’s a Problem for Cash-Strapped Cities.
- Novo plugs $500M into Ireland plant to produce Wegovy pill for markets outside US
- Esperion pays $75M-plus to acquire Corstasis and newly approved Enbumyst
- The dental workforce trends that will dominate 2026
- Federal Medicaid cuts threaten dental care access: See the potential impact by state
- Children’s Mercy raises $150M for mental healthcare
- California awards $291M to expand behavioral health housing, services
- Think bigger – Turning AI from Trends to Long-Term Transformation
- UnityPoint Health hospital names market chief nursing officer
- OhioHealth builds well-being programs to reshape caregiver culture
- Washington hospital staff vote ‘no confidence’ in management company
- U of Mississippi Medical Center restores phone lines after cyberattack
- 13 health system IT leadership moves
- UF Health taps new outpatient senior VP
- UAMS names new director of cardiovascular medicine division
- CMS’ add-on billing code boosts specialist pay: Study
- Lawmakers introduce bill to reverse Medicaid cuts, expand Medicare benefits
- Florida medical center to expand with ASC
- New Jersey woman charged with practicing unlicensed dentistry
- CMS extends hospital-at-home waivers for 5 years: What ASCs need to know
- 100+ organizations call on CMS to revise 2027 MA rates
- The retention breakthrough anesthesia needs
- Oklahoma advances interstate compact bill
- Brown University Health names new chief of cardiac surgery
- UNC Health Appalachian offers psychiatric physician training program
- Former PepperPointe Partnerships COO joins DPO
- The Smilist expands into Virginia
- Physician-led orthopedic ASC opens in Florida
- Colorado Medicaid ABA audit finds $77.8M in improper payments
- Georgia opens 30-bed forensic mental health unit to ease jail backlog
- Pennsylvania county cuts ribbon on $19.8M mental health diversion center
- UHS to roll out behavioral health revenue cycle AI tools in 2026
- UHS to roll out behavioral health revenue cycle AI tools in 2026
- In 1 state, large hospitals dominate 340B's net savings
- 15 dentists making headlines
- CMS to suspend enrollment into Elevance’s Medicare Advantage plans
- Report: Most states investing in value-based care with Rural Health Transformation Program
- U.S. Tops 1,100 Measles Cases This Year as Outbreaks Grow
- FDA To Offer Cash Bonuses for Faster Drug Reviews
- 10 providers seeking RCM talent
- PDS Health added de novos across 3 states in February
- Novant posts 4.8% operating margin in 2025
- 'One2PrEP': Gilead's 1st Yeztugo DTC ad reimagines hit song to highlight biannual dosing
- Cleveland Clinic posts $913M operating income, 5% margin — 7 things to know
- GLP-1s support heart attack recovery in rodents by relaxing tight blood vessels
- Former Optum CEO Heather Cianfrocco to depart UnitedHealth Group
- New Drug, Acoziborole, Could Boost Efforts to Wipe Out Sleeping Sickness
- Chocolate Male Supplement Recalled Over Hidden Erectile Dysfunction Drug
- Your Anesthesia Subsidy: Key Questions Every Hospital C-Suite Must Answer
- Clinician Engagement: The Operating Lever Behind Margin and Throughput
- Amid unfolding Middle East war, pharma giants keep close eye on employee safety, supply chains
- CMS set to suspend enrollment in Elevance Health's Medicare Advantage plans
- Providers urge Education Department to reconsider which jobs face stiffer student loan caps
- Kennedy adds 2 new members to CDC’s vaccine panel ahead of delayed meeting
- Kennedy adds 2 new members to CDC’s vaccine panel ahead of delayed meeting
- Urban Traffic Noise Disrupts Sleep, Affects Heart Health After One Night
- Hormone Therapy Might Be Unnecessary For Some Prostate Cancer Patients
- Benzodiazepine Use Down In U.S., But OD Risk Remains, Study Says
- GLP-1 Drugs Might Ease Chronic Migraine, Study Says
- Blood Test Reveals Alcohol-Related Liver Disease
- Telemedicine Visits Cost Five Times Less Than In-Clinic Care
- Families Defend Disability Services Amid Medicaid Cuts
- Medicaid Is Paying for More Dental Care. GOP Cuts Threaten To Reverse the Trend.
- Bavarian Nordic CEO to follow board chair out the door after failed private equity takeover
- Ascendis gains more altitude with FDA approval for dwarfism drug Yuviwel
- CDMO Quotient extends Ipsen supply pact for rare disease drug Sohonos
- Quest Diagnostics launches Google-powered AI chatbot to help patients understand lab results
- Tennr takes aim at phone call bottlenecks as it builds out automation for patient referral process
- DoseSpot, Arrive Health merge to combine prescribing tools with pharmacy, medical benefit data
- Why Digital Tool are Needed to Cope with Increasing Pressures in MedTech Innovation
- Why Digital Tool are Needed to Cope with Increasing Pressures in MedTech Innovation
- Electronics Pollution Pose Added Threat to Endangered Dolphins, Porpoises
- Flea And Tick Pills May Pose Environmental Risks, Study Finds
- ICE, ALS, Addiction Medicine, and Robotic Ultrasounds: Journalists Sound Off on All That and More
- 11 behavioral health executive moves to know
- 3 behavioral healthcare M&A deals in 2026
- Iowa dentist surrenders license
- Temple University gets approval for $3.19M rural dental clinic
- A Canadian Hospital Scoops Up Nurses Who No Longer Feel Safe in Trump’s America
- Statement on the Adoption of Final Rules Under the Holding Foreign Insiders Accountable Act
- Statement on Final Rules for the Holding Foreign Insiders Accountable Act
- State Medicaid budgets to weather $664B reduction through 2034 due to OBBBA: RAND
- Clover Health CEO said company sees opportunity in complex MA environment
- How pharma marketers are capturing the power of podcasts to connect with consumers
- Cigna's Evernorth quietly acquires hospital pharmacy CarepathRx
- Walgreens debuts virtual weight management clinic with access to GLP-1 meds
- New Obamacare Rules Could Raise Deductibles to $31K For Families
- Study Suggests One Common Amino Acid May Affect How Long Men Live
- Merck to wind down Gardasil production at N.C. plant, lay off 150-plus
- Walmart Great Value Cottage Cheese Recalled Over Pasteurization Issue
- Chris Bosh Says He’s 'Lucky To Be Alive' After Sudden Health Scare
- Patrick Kennedy: Collab with MAHA is essential to address mental health crisis
- Lilly debuts Nvidia supercomputer with fanfare and focus on escaping traditional pharma lifecycle
- Alignment CEO John Kao offers measured response to proposed 2027 MA rates
- Sanofi, Genentech, Kedrion back star-studded bleeding disorder awareness campaign
- Op-ed: Our patients deserve better safety reporting. AI could be the answer
- After CHMP nod, Moderna CEO applauds EU's 'rigorous scientific review'
- UCB's fast-growing Bimzelx leaps across blockbuster sales threshold as HS momentum builds
- Blood Test Can Predict Short-Term Survival Among Seniors
- How the Brain Learns to Have Seizures During Sleep
- Why Turning 19 Spikes Medicaid Loss for Millions
- Crash Course Might Speed Brain Stimulation Treatment For Depression, Study Suggests
- Wildfire Smoke Linked To Increase In Violent Assaults
- More Parents Are Refusing A Life-Saving Shot For Their Newborns, Study Finds
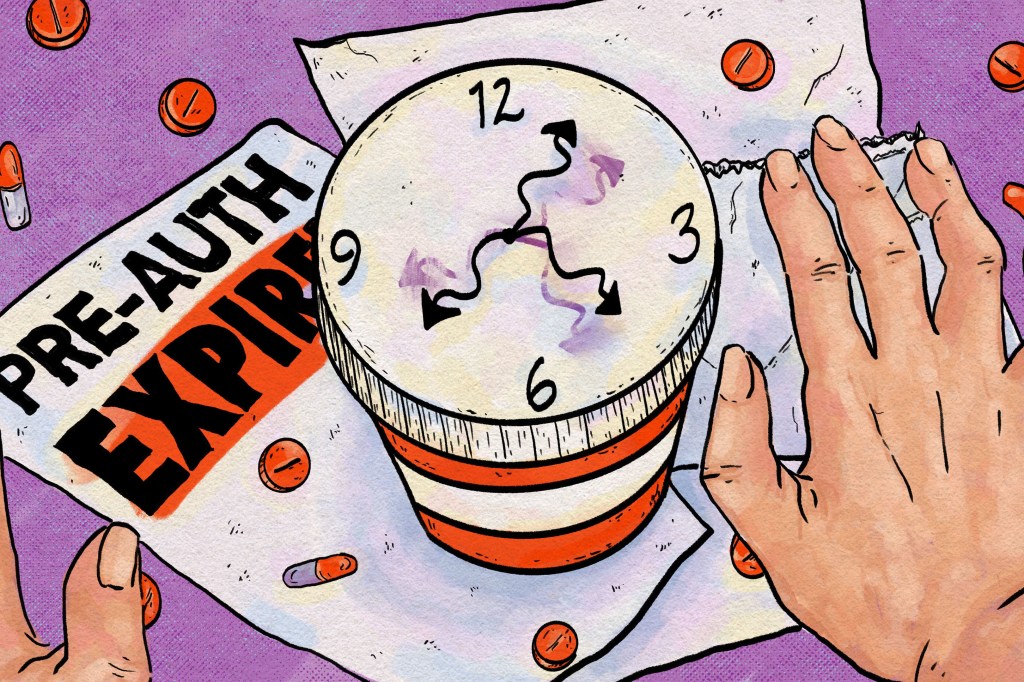
- To Avoid Care Disruptions, Know When the Clock Runs Out on Your Prior Authorization
- As SCOTUS takes on 'skinny label' review, top US lawyer sides with generics maker
- Lake Nona Impact Forum: There can't be longevity without tech
- Fierce Pharma Asia—China deal growth; Daiichi's new CMO; Astellas-Vir bispecific tie-up
- FDA Approval for BIOTRONIK Solia CSP S Pacing Lead For LBBAP
- FDA Approval for BIOTRONIK Solia CSP S Pacing Lead For LBBAP
- Catalyst OrthoScience gets FDA 510(k) Clearance of Archer® Patient-Specific Instrumentation for Shoulder Arthroplasty
- Catalyst OrthoScience gets FDA 510(k) Clearance of Archer® Patient-Specific Instrumentation for Shoulder Arthroplasty
- Smith+Nephew signs distribution agreement with SI-BONE
- Smith+Nephew signs distribution agreement with SI-BONE
- Quantum Surgical Acquires NeuWave Medical, Inc.
- Quantum Surgical Acquires NeuWave Medical, Inc.
- How Pharma is Expanding its Global Footprint to Advance Clinical Research
- Partnering to Advance Drug Delivery Innovation
- Teladoc Health reports slower growth, offers cautious 2026 outlook as it shifts telehealth model
- CFO Mark Kaye to take the helm at Carelon in leadership shake-up at Elevance Health
- Insurance groups say proposed flat Medicare Advantage rates fail to meet the moment
- Health Gorilla urges court to toss lawsuit filed by Epic, health systems
- Stryker launches Synchfix™ EVT, expanding options for flexible syndesmotic fixation
- Stryker launches Synchfix™ EVT, expanding options for flexible syndesmotic fixation
- Democrat-Led States Sue Trump Administration Over Cuts to Childhood Vaccine Schedule
- CDC Vaccine Advisory Panel To Revisit COVID Shot Safety Next Month
- Frozen Blueberry Recall Issued Across Four States for Listeria
- After delay, CDC vaccine panel sets new dates to discuss long COVID and mRNA shot safety
- Decision Criteria for Technology Commercialization of Medical Devices in 2026
- Decision Criteria for Technology Commercialization of Medical Devices in 2026
- Continuous Cardiac Monitoring: Redefining the “End” of a Clinical Study?
- Continuous Cardiac Monitoring: Redefining the “End” of a Clinical Study?

Acute prescription drug shortages will arise soon after the Senate's Prescription Drug Affordability Board and Prescription Drug Affordability Stakeholder Council are created. These are the new bureaucracies created by SB 0483, SB 0484, & SB 0485. No effort to increase supply or foster competition, only price controls:
Michigan Senate votes for board to intervene in rising drug prices
Craig Mauger - 04 October 2023Lansing — The Michigan Senate voted Wednesday in favor of establishing a new state board with the power to study prescription drug costs and set maximum caps on prices if they're determined to be too expensive for patients.
Democratic lawmakers argued the new board would help Michiganians afford medications they desperately need and counteract rising prescription drug charges. But Republicans slammed the measures, saying they were an attempt to institute government price controls and would have little impact on larger national trends.
The Senate backed the main prescription drug bill in a 20-17 vote, with all 20 Democrats in the chamber in support and 17 of the 18 Republicans in opposition. The other GOP senator, Sen. Mark Huizenga, R-Walker, didn't vote, citing a potential conflict of interest because of his background working as a consultant for the health care industry.
State Sen. Darrin Camilleri, D-Trenton, told reporters that having a Prescription Drug Affordability Board would make "a big difference in the lives of our patients and our residents." Currently, too many people are having to decide between affording food and their medication, he said during a speech on the Senate floor.
“The evidence is clear: This is a crisis that is only going to get worse," Camilleri said. "And our answer can’t be doing nothing. We must act to help our patients and help our residents."
Nationally, spending on prescription drugs increased by 16% from 2016 to 2021 — when it hit $603 billion — according to a brief from the U.S. Department of Health and Human Services. The jump was caused by "increases in spending per prescription," the federal agency found.
State Sen. Kristen McDonald Rivet, D-Bay City, said it shouldn't take a Herculean effort for people to obtain lifesaving drugs.
"We cannot allow Michiganders to die needlessly because they can't afford their prescription drugs," Rivet said.
State Sen. John Damoose, R-Harbor Springs, said prescription drug prices make "absolutely no sense." But Damoose said he voted against the bills because the problem can only be solved at the federal level.
Likewise, Michigan Senate Minority Leader Aric Nesbitt, R-Porter Township, said other states with prescription drug panels haven't experienced real savings.
"These bills seem to be less about fixing the problem and more about keeping up with the Joneses, or maybe, just keeping up with the Newsoms," Nesbitt said referencing Democratic California Gov. Gavin Newsom.
According to the National Conference of State Legislatures, seven states have prescription drug affordability boards: Colorado, Maine, Maryland, New Hampshire, Ohio, Oregon and Washington. But Newsom has touted his own efforts to combat rising prescription drug prices.
Michigan Senate Democrats introduced the three-bill prescription drug package on Sept. 12, contending the "landmark legislation" would lower health care costs for residents. Gov. Gretchen Whitmer, the second-term Democratic governor, called for an independent Prescription Drug Affordability Board during an August speech about her legislative priorities for the fall.
The new proposals would launch a board in Michigan with five members appointed by the governor. The panel would have the power to review prescription drug prices.
If the board determines there are "affordability challenges" for health care systems or high out-of-pocket costs for patients with a particular drug, it could establish an "upper payment limit" for a product, according to the language of one of the bills.
The board could consider an array of factors in making its determinations, including research on price increases, projected revenue, impacts on patients and the average patient co-pay for products. Under the bills, a prescription drug buyer or third party would be barred from purchasing a product for more than the "upper payment limit" if such a cap were set by the board.
Camilleri has said the upper payment limit would apply to all Michigan-based entities that purchase drugs meant for use in the state, including pharmacies, hospitals and the public.
But the Pharmaceutical Research and Manufacturers of America, or PhRMA, has described the proposals as "government price-setting for medications" that will "likely have long-term, harmful effects on access and the development of new, life-saving therapies."
On the other side of the bills, Dr. Eric Sullivan, chairman of the Access to Affordable Care Impact Area at Doctors for America, said the Michigan Senate's vote was"a big win for patients, seniors and families and anyone battling illness in Michigan."
"This was a vote for transparency, accountability and ensuring Big Pharma is responsive to patients in Michigan who have not been able to afford the life-saving medications they’ve needed for so long," Sullivan added.
The bills now move to the Michigan House for consideration. The House will have to approve them before they can reach Whitmer's desk.
So if this passes the MI House, we'd see prices set by the same ham-handed government that gave us COVID mandates?
Call your state reps, everybody. If you need contact info, check out the Toolbox in the pinned post.
An opinion in favor:
Opinion | Michigan needs state drug board to combat rising prices, greed
By Michigan State Senator Kristen McDonald Rivet, a Democrat who represents Michigan Senate District 35 which includes Bay City, Midland, Saginaw and surrounding townships in the Great Lakes Bay RegionOctober 19, 2023
The rising cost of prescription drugs is a crisis for Michigan families. Democrats at the state and federal levels have been working hard to tackle this issue head-on and hold big drug companies accountable.
As elected leaders, we often hear from constituents that prescription drug prices are an urgent matter that needs to be addressed, and I wholeheartedly agree. The Michigan Prescription Drug Task Force found nearly a third of residents aged 19-64 stopped taking their prescriptions because of cost.
In Michigan, we saw the cost of 500 prescription drugs rise at twice the rate of inflation during the pandemic in 2020. During a time when we’ve seen the cost of groceries and other essentials rise, the price of many prescription drugs continued to skyrocket well beyond the rate of inflation. The corporate greed by drug companies at the expense of our health and livelihoods must stop.
This is not acceptable.
Families should not have to pick between buying groceries or paying for their life-saving medication. Patients should not end up in an emergency room because they cannot afford the necessary prescriptions to manage their health conditions.
Scientific advancement has brought us so many prescription drugs that help people achieve a better quality of life. It is shameful and upsetting that these game-changing medicines remain out of reach to many because of high prices, outrageous profits and plain corporate greed.
In Michigan, we have made some strides to bring transparency to drug pricing and rein in costs. We all know there is more work to be done.
That is why I have introduced legislation as part of a package (Senate Bills 483, 484, and 485), which will create the Prescription Drug Affordability Board and ensure it is made up of nonpartisan leaders in health care economics, health policy, and clinical medicine with no personal or financial stake in the pharmaceutical industry.
There will be strict rules to prevent politicians, Big Pharma, and health care industry or special interest groups from influencing the board’s decisions.
A truly independent board is what makes this work.
We have seen recent progress at the federal level. The 2022 Inflation Reduction Act allows Medicare to negotiate prices on certain high-cost prescription drugs like insulin for seniors.
This policy marks a major win for consumers. I was disappointed, though not surprised, when the U.S. Chamber of Commerce and drug companies Merck and Bristol Myers Squibb filed lawsuits to block this law to protect industry profits over people.
The Medicare prescription negotiation program would rein in out-of-control drug prices and allow these medications to serve their purpose by getting into the hands of more Americans who need them to live and thrive.
While I am confident the law will stand up in court, these lawsuits serve as yet another reminder of the need to hold pharmaceutical companies accountable.
As the Legislature is in session this fall, advancing the PDAB legislative package that will rein in the rising cost of prescription drugs will be one of my top priorities. In the meantime, I welcome citizens struggling with the high price of prescription drugs to contact my office and share your stories.
Working together, we can tackle this critical issue and bring relief to the Michiganders struggling to keep up with the rising cost of their medicine.
Try as I might, cannot find the words "supply" or "competition" in this opinion. Fairly quickly, the government will allocate an ever shrinking supply of critical drugs.
Be prepared to demonstrate your intersectionality to the Michigan Ministry of DEI when you need pharmaceuticals in the future.
Another opinion in favor, also from BridgeMI:
Michigan doctors support state drug panel, ignore Big Pharma ads
Dr. Aisha Harris - October 30, 2023Across Michigan, physicians work hard to help our patients get access to the care they need – and that includes supporting legislation that can reduce the astronomical cost of prescription drugs. That’s why many of us are voicing our support for legislation that would establish a Prescription Drug Affordability Board (PDAB) in Michigan.
As advocates for our patients, doctors support Senate Bills 483 - 485 to create the PDAB, because this independent board, made up of nonpartisan experts in health care, can help rein in runaway prescription drug costs. Using data, this panel can set limits on the most expensive drugs, making medications more affordable for countless Michigan families.
Unfortunately, Big Pharma and its army of high-priced Michigan lobbyists are actively misleading people and even trying to fool families and legislators by explicitly representing themselves as physicians who oppose the PDAB.
Yes, you read that right.
Big Pharma, tapping its massive billion-dollar ad budgets, is using paid advertisements and websites to mislead people into thinking doctors don’t support an independent board designed to cap prescription drug costs, make them more affordable and hold drug corporations accountable for gouging our patients.
We wish to be clear. Doctors want our patients to get access to affordable medications. In Michigan, doctors support the PDAB. The Michigan State Medical Society supports PDAB. The Michigan Chapter of the American College of Physicians supports the PDAB. So do the AARP, the NAACP and many other organizations that advocate for families.
Here’s who doesn’t support Michigan’s PDAB: Large drug companies.
During hearings in September, every organization that testified against PDAB was either funded by or linked closely to pharmaceutical companies, including the National Organization for Rare Diseases and the Michigan Society of Hematology and Oncology (MSHO), whose website shows a long list of “elite” corporate sponsors that include drug giants Merck, Amgen, Abbvie, Pfizer and many more.
In 2022, Pfizer pulled in more than $100 billion in revenue; Johnson & Johnson, more than $94 billion. Merck has raked in $49.9 billion with a single drug, diabetes medication Januvia, since it launched without competition 17 years ago. Merck’s CEO Robert Davis was paid a handsome $13.72 million.
This summer, Amgen announced that it hauled in $7 billion for the quarter – more than $559 million over last year – even as patients must pay thousands of dollars for lifesaving drugs like cancer medication Enbrel, which has gone up in cost by 346 percent since 2008.
As a physician, I can say with certainty that a drug is not 346 percent more effective just because it’s 346 percent more expensive.
Meanwhile, my patients and countless more across Michigan can’t afford their life saving medications. Michiganders’ wages went up 11 percent between 2012 and 2017, yet drug costs increased by nearly 60 percent. Patients and families are constantly getting left behind, even as drug companies continue to pad their profits. Our patients are the ones who suffer.
Physicians all too often see our patients make the hard choices between paying for heat in winter or the asthma medication they need to breathe. We care for patients who were forced to ration their diabetes medication or insulin, which can cost hundreds of dollars out of pocket, putting them at risk of experiencing diabetic ketoacidosis, which can be fatal if untreated.
Michigan’s PDAB is a crucial step toward reining in out-of-control drug costs. With a robust PDAB that can keep costs in check and hold drug companies accountable when they try to gouge families, Michigan can help more people get access to affordable medications. Michigan doctors support PDAB because we took an oath to put our patients’ health and wellbeing first, unlike profit-driven drug companies.
Dr. Aisha Harris is a family physician in Flint at Harris Family Health, a direct primary care clinic. She graduated from Georgetown University School of Medicine and completed her family medicine residency at the University of Illinois in Chicago.
Still no mention of the words "supply" or "competition" in this second PDAB opinion. The fact that Big Pharma is rapacious and incompetent does not assure any level of government competence in drug pricing and distribution.
Another significant gap: proof of effectiveness.
Commissions litter the American landscape at every level of government.
If any commission, anywhere, had ever sustainably cut drug prices, surely these bill advocates would be shouting the evidence from the rooftops.
Crickets.
These three Michigan Senate bills have been idling in the House Insurance and Financial Services Committee since October 4, 2023. Chairwoman Brenda Carter may be getting ready to move them. Naomi Lopez, an adjunct scholar at the Mackinac Center for Public Policy, has some insights:
https://www.bridgemi.com/guest-commentary/opinion-who-should-control-michigans-medicine-cabinet
Opinion | Who should control Michigan’s medicine cabinet?
By Naomi Lopez - June 10, 2024In an effort to “do something” about prescription drug prices, some Michigan lawmakers want to copy an initiative passed in several states, most notably Colorado. The proposed Prescription Drug Affordability Board would set price caps on medications it deems too expensive. Before Michigan lawmakers import this misguided policy, they should consider whether they want an unaccountable board to control the state’s medicine cabinet.
The potential ramifications of handing over decisions about access to prescription medicines to a new unelected state board are huge. Similar proposals were recently vetoed in Virginia. And it failed four times in the Wisconsin Legislature, including getting voted down again last month. Before Michigan follows in Colorado’s footsteps, the public should be asking lawmakers five important questions.
1. Why are advocates for patients with rare diseases, who are often most impacted by drug pricing decisions, excluded from the board’s represented members? The proposal requires a patient advocate but the patient groups often facing the cruelest diseases and fewest treatment options are left without a voice.
2. Why does Michigan’s proposed law not ban the use of “quality-adjusted life years,” a controversial metric that devalues the lives of the elderly, those with physical and mental disabilities, and chronic conditions? The use of this measure has already been outlawed in the federal Medicare program and should not be allowed here. Michigan lawmakers must ensure that they don’t hard code discriminatory treatment against the most vulnerable patients in creating this board.
3. Who will get the “savings” the board is tasked to create? There are no guarantees or provisions that any savings achieved through price caps and restrictions will be passed on to consumers. The result could be zero financial relief for patients with access to fewer treatment options.
4. What is the recourse for vulnerable patients subject to the board’s decisions? Colorado has targeted a popular arthritis medication for potential price controls and restrictions. According to Michigan's own health data, arthritis is more prevalent in the state than the national average. In addition, the disease burden of arthritis can also affect the ability to work, may disproportionately affect those in the manual trades and affect those who are older. The repercussions of ceding authority over important health care decisions to an unelected and unaccountable board will be far-reaching.
5. Will Michigan lawmakers themselves be subject to this board? Lawmakers serving in the Michigan House may participate in a state-sponsored plan that is governed by federal law. As proposed, this health plan would be exempt from a prescription board’s decisions. Before Michigan lawmakers hand over power and authority for critical health care decisions, they should be willing to operate by the same set of rules and consequences that they would impose on their constituents.
While the interest to reduce drug prices is commendable, a willingness to move forward without protecting patient access to treatments and with no accountability to citizens is a perilous prescription. Programs cannot be evaluated by their intentions. Outcomes matter and they matter even more so where patient well-being is concerned. Michigan’s lawmakers should learn from others’ mistakes and dangerous examples, not double down on them.
Outstanding article, and great action items!
The Michigan Senate revived the Prescription Drug Affordability Board concept, this time with a Republican's support:
Prescription price cap plan passes Michigan Senate as Dems decry ‘exploitation’
By Simon D. Schuster - April 24, 2025* Michigan’s Democratic-led Senate approves plan to create Prescription Drug Affordability Board
* Board could cap prescription prices if members determine costs are preventing patients from receiving deeded care
* Pharmaceutical industry and most Republicans oppose plan, which one lawmaker calls a ‘Soviet-style price-fixing scheme’Michigan Democrats are taking another stab at creating a government board intended to rein in prescription drug costs, this time with slightly more Republican support but an uncertain path forward in the GOP-controlled House.
Bills that could empower state government to cap prices on expensive prescription drugs cleared the Michigan Senate on Thursday, with one Republican joining majority Democrats to support the creation of a Prescription Drug Affordability Board.
Democrats have pushed the measure as a means of directly lowering the cost of expensive medications. Many Republicans, however, have criticized it as an unproven means of meddling in a free market better left untouched.
“This board is not about stifling innovation. It's about stopping exploitation that is happening now,” said Sen. Sue Shink, D-Northfield Township.
The legislation would create a five-member board and a separate 21-member council that could review prescription drugs for cost and affordability, and set caps on their cost if they determine the cost of the medication is preventing patients from receiving the treatment they need.
Private insurers and Medicaid would have to comply with the limits set by the board, which would be appointed by the governor and receive recommendations from a council of stakeholders.
The pharmaceutical sector remains strongly opposed, with one industry group calling the proposed board “a disaster for patients.”
The legislation would give “unelected bureaucrats a veto pen over the medicine or the treatments doctors prescribe and patients need,” Stami Turk, the Director of Public Affairs for PhRMA, said in a statement.
Senate Minority Leader Aric Nesbitt, R-Porter Township, called it a “Soviet-style price-fixing scheme” and a “bureaucratic boondoggle” that hasn’t worked in other states.
But supporters see the proposal as an urgently-needed intervention amid rising healthcare costs.
Michiganders “are rationing their medication, skipping doses or going without it altogether” due to high costs, said Sen. Darrin Camilleri, D-Brownstown Township.
Minnesota, Colorado, Washington and Maryland have created similar boards with prescription drug price-setting powers. A 2024 review of their boards in the journal Health Affairs found the long-term impacts of those price controls “on benefit design, patient access and innovation are not yet known.”
Gov. Gretchen Whitmer first called for the creation of a Prescription Drug Affordability Board in an August 2023 speech, and lawmakers introduced a proposal soon after. But the legislation failed to gain traction in the Legislature when Democrats controlled both chambers.
The prior version of the proposal passed the Senate in October 2023 along party lines. Democratic House members said they had “no explanation” why the House never took up the legislation when their party controlled the chamber. Now, however, Republicans control the House.
“Last time, I was persuaded by the idea that the market should determine the cost of (prescription drugs),” said Sen. John Damoose of Harbor Springs, the lone Republican supporter for the package.
“The more I learned, the more apparent it became that calling the prescription drug market a free market is a total farce.”
Getting the GOP majority in the House to come around appears to be an uphill battle. Democratic legislators in the House said they have yet to convince any Republicans to come forward to support the bills, but have only begun to try.
Speaking with reporters Thursday, House Speaker Matt Hall, R-Richland Township, called it a “very controversial proposal.”
While Hall said he “supported bipartisan solutions” for lowering drug costs, he referred the Senate package to the Government Operations Committee, a panel where legislation is often sent to die.
“I think that if Republicans in the House are smart, they will make this bipartisan and negate this as a talking point in the next election cycle,” said Rob Davidson, an emergency physician from West Michigan and former Democratic congressional candidate who supports the legislation.
Morning Brew, a left-leaning daily e-news source, brings practical skepticism to its overview of state UPLs (upper price limits).
https://www.healthcare-brew.com/stories/2025/04/16/state-drug-pricing-boards-gaining-momentum
State drug-pricing boards are gaining momentum
Experts say more states may follow after judge dismisses Amgen lawsuit.
Now that the US government is negotiating drug prices directly with manufacturers, states want to get in on the action, too.
These efforts vary by state, but generally involve creating a board to review drugs’ affordability and sometimes setting upper price limits (UPLs). While none have implemented UPLs as of April, as the idea gains momentum, there are questions about UPLs and boards’ legality, practicality, and whether they will actually lower costs for patients.
A legal first
Colorado, for instance, enacted legislation to establish a prescription drug board in 2021, and drug prices have continued to rise since then. Over the last year, that board reviewed five drugs and declared three unaffordable, including biopharmaceutical company Amgen’s Enbrel, a biologic which treats autoimmune disorders like rheumatoid arthritis. The state then moved to set a UPL for “all purchases and payer reimbursements” in February 2024.
Enbrel can cost about $8,000 a month without insurance, according to GoodRx, and cost insurers in Colorado $46,772 per patient in 2022, according to the Colorado All Payer Claims Database—though Amgen advertises a co-pay program promising insured patients can pay “as little as $0 out-of-pocket for each dose.”
Amgen responded by suing the state in March 2024—the first legal challenge to this broader concept—alleging this move was unconstitutional. On March 28, a judge ruled that the company lacked standing and threw the case out, creating a path for Colorado to continue with its board.
Amgen moved to appeal the ruling in early April.
“We continue to have significant concerns with the board’s flawed policy and procedures during the rulemaking process to set an upper payment limit…Price controls will not meaningfully address affordability at the pharmacy counter and will instead create new access barriers for patients,” Amgen spokesperson Kelley Davenport said in an emailed statement to Healthcare Brew.
The Colorado Division of Insurance, which oversees the board, did not respond to a request for comment, but Isabel Cruz, policy director at the Colorado Consumer Health Initiative, sent a statement to Stat News celebrating the ruling as a promising step forward.
“Drugs don’t work if people cannot afford them,” she wrote.
Unanswered questions
Zachary Cook, VP of Healthcare Policy for government affairs consulting firm Stateside Associates, told Healthcare Brew via email he expects the ruling could inspire other states to create boards of their own.
Starting with Maryland in 2019, at least nine states have implemented prescription drug affordability review initiatives, including boards, according to a 2024 blog post from the National Alliance of State Pharmacy Associations. States like Michigan are debating implementing drug affordability reviews.
Colorado’s review board is set to start Enbrel rulemaking during a May 23 meeting.
This concept has inspired mixed reactions and plenty of questions. Patient advocacy organizations like the American Cancer Society Action Network (ACS CAN) and the Cystic Fibrosis Foundation have said that boards could potentially help drive down costs, but have the potential to hurt patient access if they do not center patients in the design process.
For instance, if manufacturers think a new drug could be subject to a UPL, they might jack up launch prices to compensate, ACS CAN said in a recent report. Manufacturers could also choose to stop selling a drug in a state with a low UPL or eliminate patient assistance programs to make up for lost profits.
“The impact of UPLs could be positive, negative, or a mix of both, depending on how they are implemented,” the report read.
Cook echoed this idea.
“There are many unknowns as to the effects of a board-implemented UPL on drug cost and patient access,” Cook said.
Michael Abrams, a managing partner at healthcare consulting firm Numerof & Associates, told us he agreed the approach raises questions. (He disclosed his company has worked with Amgen in the past but does not currently.)
“As more and more states set upper price limits on more and more individual drugs, it becomes a huge administrative burden, both for the state and for the pharmaceutical companies, and that simply adds to everybody’s overhead,” he said.
He added that many patients don’t pay the list price, and it’s unclear whether UPLs will actually result in lower costs for consumers.
“This general approach just doesn’t seem to be viable,” he said.
Caroline Catherman joined Healthcare Brew in July 2024 after three years as a health reporter for the Orlando Sentinel. Her work has appeared in outlets including CNN, Science Magazine, and The Chicago Tribune. She holds a master’s in health, environment, and science journalism from Northwestern University and degrees in psychology and English from Emory University, where she was first author on a public health study.
Get MHF Insights
News and tips for your healthcare freedom.
We never spam you. One-step unsubscribe.